Translate this page into:
Neonatal innovations in resource-limited settings
-
Received: ,
Accepted: ,
How to cite this article: Agarwal N, Kumar R, Gupta G. Neonatal innovations in resource-limited settings. Karnataka Paediatr J 2021;36(2):82-6.
Abstract
In the year 2000, Millennium Declaration was signed by the world leaders to reduce the under-5 mortality rate by two-thirds from the baseline figure in 1990. Millennium Development Goal 4 was replaced by the Sustainable Development Goal (SDG) in 2015. Reduction in the neonatal mortality, which accounts for majority of the deaths in children under the age of 5 years, was an imminent goal of SDG. Despite these initiatives, the current trends in neonatal mortality are far away from the expected targets. To curb the rate of neonatal mortality, the neonatal services are expanding in India at a rapid pace. To bridge the gap between the availability and accessibility to the health care technology between the developed and developing countries, the current focus is toward the development of low-cost and effective technological innovations in neonatal care and ensuring their patenting and effective publicity. This should facilitate the translation of innovations into mass production and availability for practice with significant effect in low- and middle-income countries. Generation of evidence will increase the acceptability of these innovations by demonstrating their benefit over the currently available technologies. Fortuitously, India has developed many innovations in the neonatal health care. However, majority of the neonatologists are still unaware of the existing technological solutions, and the ways to optimally utilize them. This review is, therefore, an attempt to recognize such low-cost, effective, and sustainable innovations done in the field of neonatology, over the past few decades.
Keywords
Cost effective
India
Innovation
Neonatology
Technology
INTRODUCTION
Globally, there is a rise in the neonatal mortality rate (NMR) from 40% of all child death’s under-5 years age, in the year 1990 to 47% in the year 2019.[1] This suggests minimal or negligible advancement in the field of neonatal care over the past few years. Neonate and their mothers are the most vulnerable population, particularly in the low- and middle-income countries (LMICs). In India, the rate of decline of NMR is slower and lags behind the infant mortality and under-5 mortality rates. Recent data suggest that worldwide, India ranks the highest in NMR.[2]
In an attempt to curb the rate of neonatal mortality, the neonatal services are expanding in India at a rapid pace. Given the high cost involved in setting up a tertiary care neonatal intensive care unit (NICU), heterogeneity in the quality of care is imminent across the nation. To overcome this disparity and to bridge the gap between the availability and accessibility to the health-care technology between the developed and developing countries, the current focus is toward the development of low-cost and effective technological innovations in neonatal care. Fortuitously, India has recently witnessed many such innovations in the neonatal health care.
INNOVATION IN LMICs
Over the past few years, technology has leaped into the medical care to facilitate better and improvised management. However, these technological innovations are mainly limited to the industrialized world.[3] Due to the dearth of technology in the developing countries, a large majority of neonatal and maternal deaths occur in the underdeveloped/developing nations.
Recently, due to an increasing interest in global health, there is an increasing demand of technology “appropriate” for the resource-limited settings. The World Health Organization defines the “appropriate technology” as “scientifically valid, adapted to local needs, acceptable to both patient and health-care personnel and that can be utilized and maintained with resources the community or country can afford.”[4]
However, majority of the neonatologists are still unaware of the existing technological solutions, and the ways to optimally utilize them. This review is, therefore, an attempt to recognize such low-cost, effective, and sustainable innovations done in the field of neonatology over the past few decades.
INNOVATIONS SO FAR!
The innovations done range from simple bedside medical devices to ventilation assisting devices. Many of these are available in public domain accessible to all, while others are available on other databases still requiring peer-review and scrutiny by practitioners. As there is no ready list of innovations developed in India in neonatology, the present paper is an effort to enlist the innovations, whose details could be obtained. In no way, it is a comprehensive or an updated list of the innovations. For the ease of understanding, these innovations have been grouped as those involved in patient care and others that are evolved to train the medical students.
Patient care
Respiratory care
Girisam Endotracheal and Auxiliary Tube Fixator
It was developed in the year 1995, as a safe, effective, and an atraumatic means of fixing endotracheal tube (ET), [Figure 1]. Conventional methods of fixing the ET are associated with an increased risk of facial abrasions with secondary nosocomial sepsis. This innovation ensures zero tube mobility and helps in reducing skin abrasion and sepsis. The innovation is under the process of patenting.

- Girisam Endotracheal and Auxiliary Tube fixator.
Warmidified oxygen
Dry or even humidified oxygen may not get warmed up by natural bodily mechanisms because of sickness, and hence may be less beneficial and even harmful. To overcome this concern, concept of Warmidified oxygen delivery was developed in the year 1996, using standalone humidifiers, to ensure both humidification and warmidification.
Water trap for humidified oxygen through oxygen hood
This was designed to tackle the problem of water dripping on baby’s face from the oxygen hood, [Figure 2].
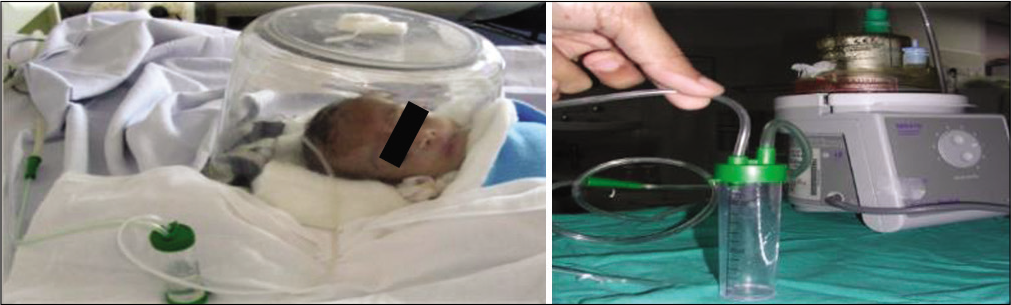
- Water trap for humidified oxygen through oxygen hood.
Split bubble continuous positive airway pressure (bCPAP)
To multiply the use of single bCPAP to two neonates, an attempt to split non-invasive respiratory support system was developed, Verma et al.[5] It used a T-piece splitter to split bCPAP. It is a technically simple, feasible, and reliable strategy tested in a simulation model.
Cardiovascular care
Head pulse oximetry
This pilot project was initiated in the year 2000 to address the fallacy of false oximetry readings, in the presence of poor perfusion or arm bandages. The available pulse oximeter probe was used for head pulse oximetry, [Figure 3].

- Head pulse oximetry.
Asepsis
Alcohol dispenser for hand disinfection
It was conceptualized in the year 1995, to reinforce hand disinfection in economic and feasible manner so that each neonatal bed could have a disposal plastic bottle filled with methyl spirit that could be hung, [Figure 4].
- Alcohol dispenser for hand disinfection.
Aseptic intake output chart
This was developed in the year 1995, to provide intake output charts at bedside without compromising asepsis, this involved creating an assembly of sterile plastic board with autoclaved chart papers with disinfected pen, being hung on each bed, [Figure 5].
- Aseptic intake output chart.
GAARIEP: Indian Innovation of caps and personal protective equipment
COVID-19 pandemic has brought an unprecedented crisis across the globe. There has been a shortage of adequate number of face masks and protective gears. To tackle this problem, protective gears were designed using the easily available materials in the NICU.[6]
Jaundice management
Unavailability of effective phototherapy units poses an increased risk of kernicterus and double volume exchange transfusions. Efforts were made to use Isabgol husk to reduce the enterohepatic recirculation of bilirubin.
Routine neonate care
Heat shields for neonates
Commercially available heat shields are not only costly and also not freely available. [Figure 6] depicts free, easily available, disinfectable, disposable innovative alternatives of heat shields in neonates. It has been made by bleaching used radiograph films.

- Heat shields for neonates.
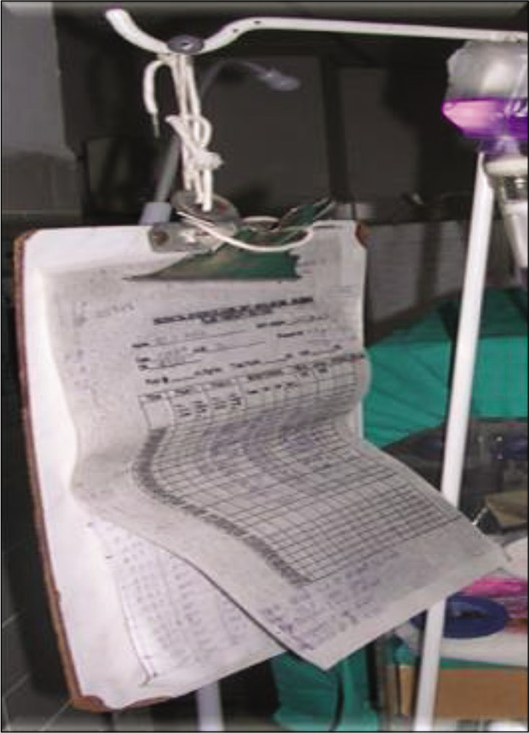
Incubator
Col Vishal Tewari, in the year 1996, designed a simple, light, disinfectable, non-battery or electricity operated incubator using cling wrap, humidifier, and air probe to warm micropremies, in an incubator-like environment using air mode, [Figure 7].
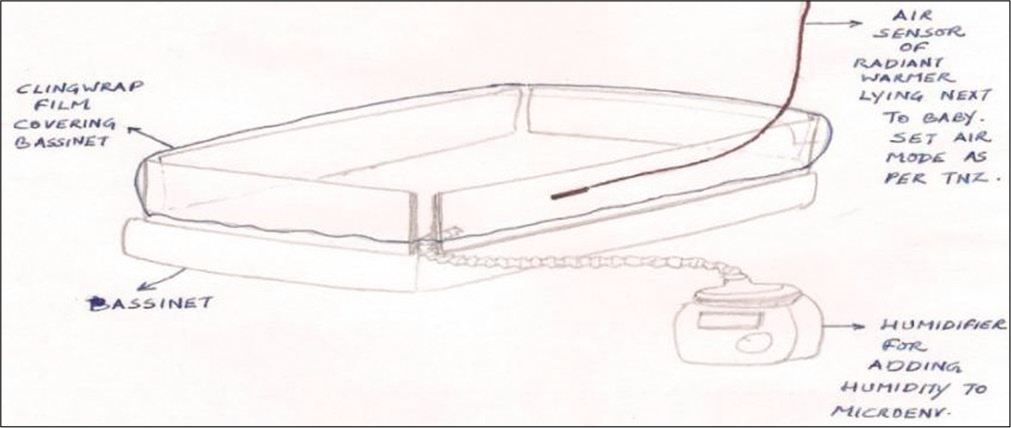
- Open care converted as an incubator.
Transport incubator
A simple transport incubator was developed with a lightweight canopy, which could be carried easily. The mechanism of heating involved an exothermic reaction producing chemical filled bags. This incubator remained appropriately warmed for 3–4 h and was easy to disinfect. This innovation won the best innovation award of NNF.
Girisuz syringe feeding T
To address the transition of feeding from gavage to nipple feeds, syringe feeding was conceptualized, as shown in [Figure 8].

- Syringe feeding.
Clinical volumetry
Used mucus traps were used as inexpensive/disposable volumetric collector device for various body fluids, [Figure 9].

- Mucous trap for urinary volumetry.
Effects of musical intervention on vital parameters of neonates
Sounds of different frequencies from different sources example, Garbh-Sanskar music, female singing voice, classical instrumental music, and recorded human heart sounds with background of lullabies were played in NICU. Changes observed in vital parameters are depicted in the graph below, [Figure 10]. The graphs show encouraging stress reduction effects on vital parameters.
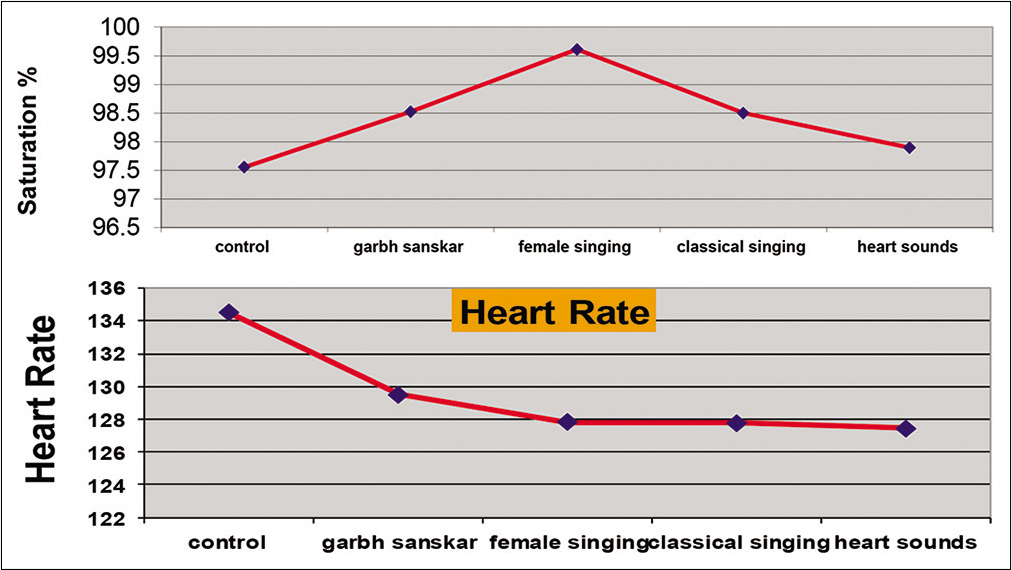
- Effects of musical intervention on vital parameters of neonates.
Training innovations
Various innovations act as simple affordable simulators to help acquire skills. Some of these are enumerated below:
“GirAash” Needle Cricothyrotomy trainer
Pericardiocentesis trainer
Peritoneal dialysis trainer
Girebu PICC Trainer
PICC insertion trainer
Intraosseous trainer
Umbilical vessels catheterization trainer
Suprapubic cystostomy trainer
Asvini formula for inotropes infusion calculation
Girish’s Calf sign for early diagnosis of hemodynamically significant PDA
Medical applications available on smartphones with cardiac sounds were used to take examination of UG and PG students
Ek Pahal: It is a 7 min human attributes developer program consisting of taking vows and practicing pranayama.
Limitations
Many of the innovations described above are yet to be published.
CONCLUSION – THE WAY FORWARD!
To decrease the neonatal mortality in LMIC countries, the most important and may be the only way ahead is to innovate and motivate the use of locally available resources as effective alternatives.
Creating evidence can contribute to increase in the acceptability of these innovations by demonstrating their benefit over the currently available technologies.
We believe that this article would serve the purpose of accelerating the rate of innovation diffusion/translation of the existing innovations of LMIC countries. It is also suggested that concerted facilitatory efforts must be made to help develop and propagate innovations. Some of the following methods are considered important.
Encouraging the formation of a nation-wide neonatal innovation registry
Inspiring and stimulating clinicians, or budding neonatologists to invent and/or innovate, by awarding or recognizing the innovators at various platforms
Inclusion of innovation and patents in the syllabi of medical and nursing education
Facilitating the process of patenting.
It is hoped that this article will serve as a catalyst in setting up a new script for innovations.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- UN Inter-agency Group for Child Mortality Estimation. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. Lancet Glob Health. 2019;7:e710-20.
- [CrossRef] [Google Scholar]
- Mapping neonatal and under-5 mortality in India. Lancet. 2020;395:1591-3.
- [CrossRef] [Google Scholar]
- High and rising health care costs Part. 1 Seeking an explanation. Ann Intern Med. 2005;142:847-54.
- [CrossRef] [PubMed] [Google Scholar]
- A Glossary of Terms for Community Health Care and Services for Older Persons Japan: World Health Organization Kobe Centre; 2004.
- [Google Scholar]
- Bubble CPAP splitting: Innovative strategy in resource-limited settings. Arch Dis Child. 2021;106:137-40.
- [CrossRef] [PubMed] [Google Scholar]
- GAAREIP: Indian innovation of caps and personal protective equipment. J Neonatol. 2020;34:24-7.
- [CrossRef] [Google Scholar]






