Translate this page into:
Oscillometry – The future of estimating pulmonary functions
-
Received: ,
Accepted: ,
How to cite this article: Gupta N, Sachdev A, Gupta D, Gupta S. Oscillometry – The future of estimating pulmonary functions. Karnataka Paediatr J 2020;35(2):79-87.
Abstract
The prevalence of asthma is increasing rapidly, worldwide, due to changing gene-environment interactions. The rate of rise is more in resource poor nations due to lack of knowledge and non-availability of expertise. Monitoring of lung functions is mandatory for diagnosis and further management of asthmatic patients. Spirometry, the widely available investigation, is the gold standard test used for mapping pulmonary dynamicity. It has got its own limitations in the form of operational difficulties in children, the elderly, and in those with neuromuscular or behavioral issues. In the current era of COVID-19 pandemic, the utility of spirometry has been further restricted to selected cohort only, due to potential risk of viral transmission during the procedure. Oscillometry technique has been used previously, to monitor lung functions, with promising results. Ultrasonic waves of various frequencies accompany the tidal breath of patients and respiratory impedance is calculated by measured pressure and flow signals from exhaled breath. The results are interpreted in the form of resistance, reactance, resonant frequency, and reactance area. Various manufacturers have developed different mechanical models with slight variation in impulse pattern till date. There are certain distinct advantages of oscillometry over spirometry. Being tidal breath-based maneuver, it is more child friendly. People with neuromuscular weakness, cognitive limitations, and the elderly can easily perform it with only minor understanding and effort. Oscillometry is more sensitive than spirometry in detecting peripheral airway diseases. Post-bronchodilator reversibility can be evaluated by comparing with the baseline respiratory characteristics. Their utility in restrictive diseases and vocal cord dysfunction has also been explored. Less aerosol generation during the normal tidal breath is another advantage of oscillometry, over spirometry needing forceful efforts, which makes it more suitable for use in viral pandemic situations for monitoring patients with both asthma and pneumonia. More research is needed, in various geographic locations and heterogeneous populations, to devise the normative data of oscillometric parameters. Simultaneously, there is an urgent need for standardization of available machines at global platform.
Keywords
Oscillometry
Spirometry
Pulmonary function test
Respiratory impedance
COVID-19
INTRODUCTION
Allergic disorders are increasing worldwide with substantial affliction toward developing countries.[1] The current global prevalence of diagnosed asthma cases is 300 million.[1] In India, about 30% of the population is affected by some form of allergy.[2] Asthma prevalence has increased many folds over the past 6 decades and is currently influencing 15% of people in Indian capital.[3]
As per a recent estimate, approximately half of the children present to a physician with at least one episode of wheezing by their sixth birthday.[4] These figures are underestimate of real quantity due to lack of awareness among health-care providers and non-availability of reliable diagnostic modalities in resource poor nations.[3] Demonstration of reversible airflow obstruction is desired in any patient with features of chronic airway inflammation (such as recurrent wheeze, breathlessness, chest tightness, and cough of variable intensity) for making a diagnosis of asthma.[5] Spirometry is considered gold standard technique for demonstrating airway reversibility in suspected cases.[6] Although universally accepted, this modality has practical difficulties such as requirement of patient cooperation and forceful respiratory efforts.[6] It is cumbersome in young children, the elderly, patients with neuromuscular weakness, post-cardiothoracic surgery, and those with learning problems.[7,8] Finkelstein et al., in a multicentric survey, demonstrated that only 21% of 671 primary care physician used spirometry, due to operational dilemmas.[9] About 28% of people were either missed or overdiagnosed in another study using this tool.[10] Inability to reliably diagnose peripheral airway and parenchymal diseases are other shortcomings of this age-old technique.[10] Spirometry is not dependable in under-five wheezers.[5] With the emerging global problem of asthma, we urgently require a competent method which can overcome many of these shortcomings. An ideal lung function test should be possible at any age, safe, simple to perform, reproducible in different circumstances, and sensitive enough to detect minor changes in respiratory mechanics.[11]
Any technique based on tidal breathing would be ideal, especially in pediatric age group, where the cooperation expected from the subjects is minimal. Among the various available diagnostic modalities, some are oscillometry, interrupter technique, and body plethysmography.[12] Oscillometry seems a reasonable option to determine pulmonary mechanics in patients who are unable to perform spirometry.[13] It works on the principle of moving sound waves over tidal breath during the respiratory cycle. Resistance and reactance are calculated from measured changes in pressure and flow at different frequencies. Oscillometry is better in children and can provide additional information in adults for monitoring lung functions compared to spirometry.[14] Oscillation principle has been used previously in both pre-school and school-aged children to assess lung functions.[15] Gupta et al. have recently demonstrated airway reversibility using this technique in children as young as 2 years of age.[16] Patients with physical and cognitive limitations were also able to perform this maneuver convincingly.[17] Komarow et al. have explored its utility in identifying vocal cord dysfunction.[18] Another key highlight is reduced aerosol generation in oscillometry, which makes it a safer alternative in COVID-19 pandemic.[19]
HISTORICAL PERSPECTIVE
Oscillations were first used to quantify the mechanical behavior of respiratory system by Dubois et al. in 1956.[13] The approach commonly known as forced oscillation technique (FOT), in which airway characteristics in the form of impedance were monitored using sound waves of various frequencies. There have been several modifications in FOT over the past 6 decades with regard to configuration, oscillation type, frequencies, and assessment of airway parameters.[20] One such development, known as impulse oscillometry (IOS), was demonstrated by Michaelson et al. in 1975 using multiple frequencies at one point of time.[21] Oscillometry provides a detailed description of pressure-flow relationships over discrete frequencies. This provides a better insight about resistance and reactance of respiratory system than conventional spirometry.[8]
TYPES
Depending on the type of oscillation signals used, this technique can be classified as:[22]
Monofrequency using single sinusoidal pressure waveform
Pseudorandom noise (PRN) where impulses of several frequencies are simultaneously applied
IOS in which recurrent impulses (square waveform) applied at a fixed frequency of 5 Hz.
Single frequency impulses are useful for monitoring patients with sleep apnea or those on mechanical respiratory support (ventilation or continuous positive airway pressure). PRN FOT impulses are widely used for monitoring various obstructive (asthma, bronchitis, and emphysema) and restrictive (interstitial lung disease, pulmonary fibrosis, and thoracic wall abnormalities) diseases. Intrabreath changes are better defined using recurrent impulses. Dandurand et al. have demonstrated that devices with PRN FOT signals are better in measurement of peripheral lung characteristics, than others, when subjected to higher mechanical load.[23]
The commonly used commercially available machines working on PRN impulses are Wave Tube, TremoFlo C-100, MostGraph-02 prn, and Resmon Pro, whereas Master Screen IOS and MostGraph-02 imp work with recurrent impulses.[23] The two most commonly available FOT models, Master Screen IOS and Resmon Pro, use 5, 10, and 20 Hz and 5, 11, and 19 Hz frequencies, respectively, to study the airway mechanical properties.[23]
PRINCIPLE
Oscillations of different frequencies are used to study respiratory impedance in FOT. The technique requires only passive cooperation from the patients for the evaluation of lung functions.[24] Respiratory impedance (Z) is a measure of resistive, inertial, and elastic forces of lungs and thoracic cage.[25] Sound waves of multiple frequencies, generated by a loud speaker, are superimposed over tidal breath of subjects through the respiratory system [Figure 1].[8]
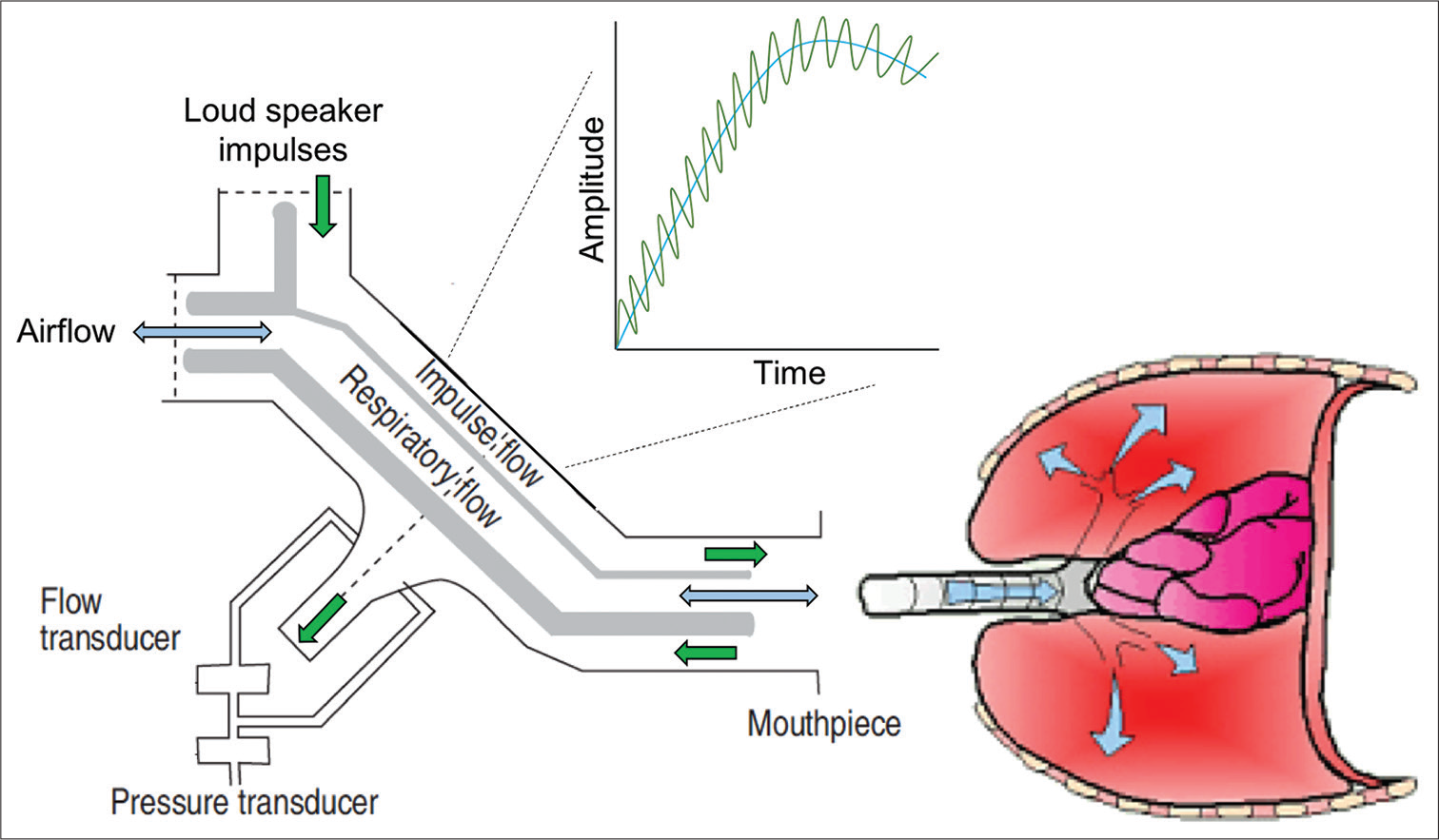
- Principle of oscillometry. Sound waves (green) are superimposed over the normal tidal breath (blue) during respiration. Transducers measure the pressure and flow during exhalation for individual frequency which is utilized to calculate impedance of the respiratory system.
These sound waves, being the mini pressure waves, cause subtle pressure changes in the airway which leads to change in airflow.[24] Smaller frequencies (2–4 Hz) can travel till the depth of lung peripheries, whereas higher frequencies (>20 Hz) reach to proximal conducting airways only.[26] Middle range frequencies (5–20 Hz) are commonly used in clinical practice to determine respiratory characteristics [Figure 2] using fast Fourier transform technique.[14] Frequencies less than 5 Hz get easily altered by harmonics of the normal breathing,[26,27] whereas larger frequencies (>30 Hz) cause subjective discomfort and are affected by shunting properties of upper airways.[26,28]
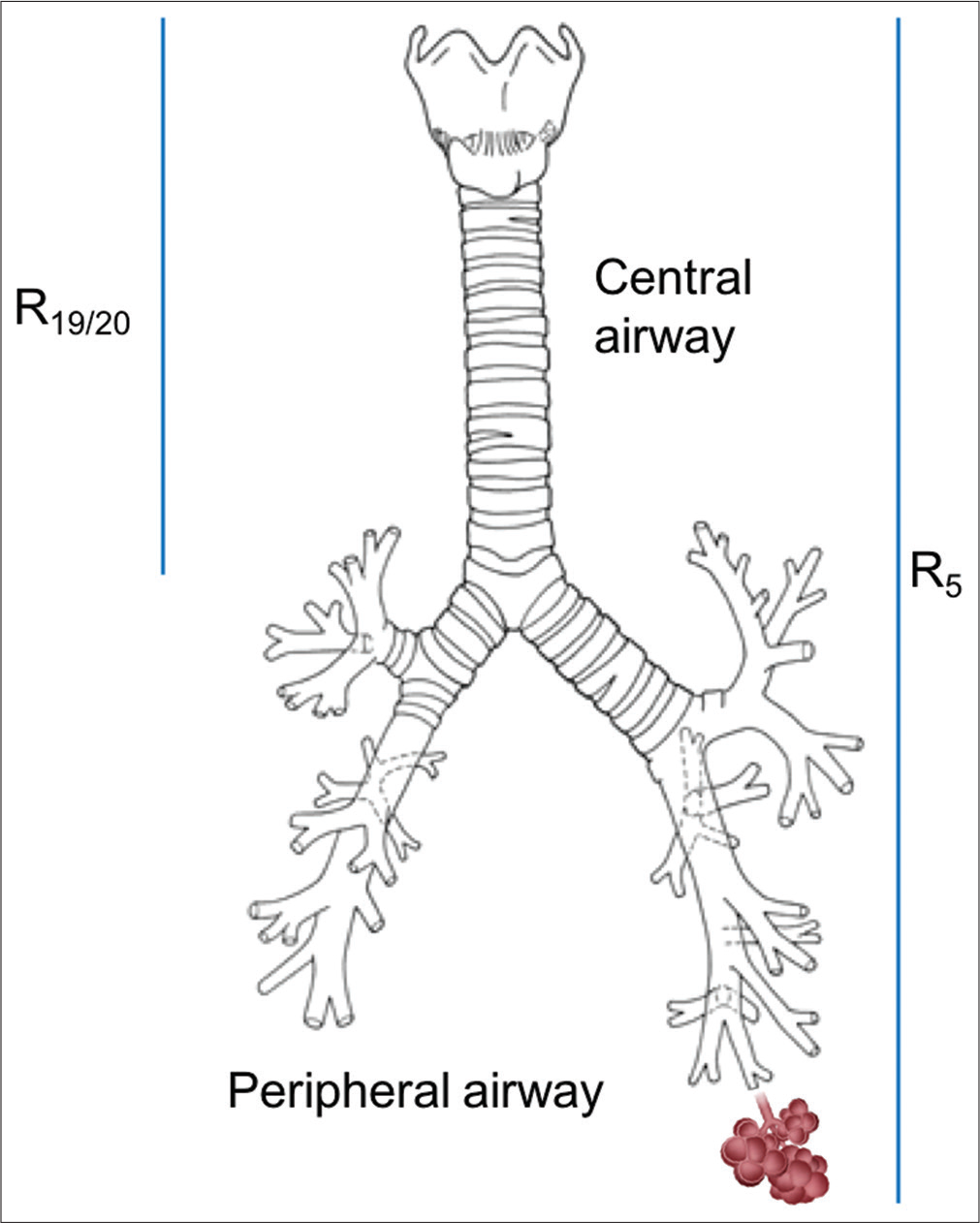
- Impulses of various frequencies traveling through airway. Smaller frequency sound waves (5 Hz), being more energetic, travel till the farthest point of respiratory system, that is, alveoli. Higher frequency (20 Hz) remains in the central airways depicting the characteristic of respective part.
The sound wave signals of pressure and flow are separated from the breathing pattern, by signal filtering mechanism, while returning from lungs during exhalation. The complex ratio of sinusoidal pressure (P) and flow (Q) for individual sound wave frequency, as determined by the pressure and flow transducers (pneumotachograph) at the mouthpiece, informs about the impedance of various segments of the respiratory system [Figure 1].[25] Impedance is calculated at discrete frequencies by ohm’s law.
Where Z – Impedance, P – Pressure, Q – Flow, ω – oscillation frequency function, f – frequency
Measured impedance (Z) is the sum of opposing forces in the respiratory system, resistance (R), and reactance (X). Z, calculated at individual frequency, informs about the mechanical properties of respective portion of airways [Figure 2].
TERMINOLOGY
-
Impedance (Z) – It is defined as sum total of all the resistive, inertial, and elastic forces of respiratory system which a pressure impulse has to encounter during its travel through the respiratory system. It can be represented by a combination of resistance (R), a real force, and reactance (X), an imaginary component. Resistance and reactance are associated with energy dissipation and storage, respectively[25]
R – Resistance, j – unit imaginary number defined as √-1, and X – Reactance
Resistance (R) – It is a measure of opposition to airflow. It is directly proportional to length and inversely proportional to fourth power of radius of conducting tubes. Resistance measured at a particular frequency (f) is labeled as Rf, for example, R5 is resistance detected at 5 Hz. Rf includes the resistance of oropharynx, larynx, trachea, large and small airways, lungs, and chest wall tissue
-
Reactance (X) – Reactance can be understood as rebound resistance produced by distensible airways.[29] It is an imaginary component of impedance, which is defined by balance between inertance (I) (positive force) of conducting airway and capacitance (C) (negative force) of pulmonary parenchyma. Capacitance is in inverse correlation with elastic properties of lung
Where X – Reactance, I – Inertance, E – Elastance, and C – Capacitance
Reactance measured at a particular frequency (f) is labeled as Xf, for example, X5 is reactance at 5 Hz. At lower frequency, reactance is negative due to predominant capacitative forces, whereas it becomes positive toward higher frequencies, with major contribution from inertial forces [Figure 3]
Resonant frequency (Fres) – It is the arbitrary frequency number at which capacitative and inertial forces equalize and reactance becomes zero [Figure 3]. Elastic forces dominate below Fres, whereas airway inertance plays major role above Fres.[29] Fres is usually higher in children and reduces with age
Reactance area (Ax) – It is the triangular area limited by Fres (on right side) and reactance at 5 Hz (on left side) [Figure 3]. Ax provides information regarding peripheral airways and lung parenchyma. It is more sensitive parameter than Fres and X5 (in descending order) for the detection of small airway obstruction as well as to document the bronchodilator reversibility
Coherence – It is a quality control parameter which reflects the reliability of oscillometry maneuver. The value depends on relative comparison between input (flow) and output (reflected pressure) in the respiratory system.[30] Coherence values of >0.8 at 5 Hz and >0.9–1 at 20 Hz are considered satisfactory in adult subjects but cutoffs are yet to be validated for children.[15,31] The potential problem in relying on coherence is varied approaches used for calculations leading to different values by different manufacturers. Coherence values are reduced in pathological conditions or due to improper technique including swallowing, glottis closure, tongue causing airflow obstruction, and irregular breathing during the oscillometry maneuver.[32] High coherence values cannot rule out measurement errors or artifacts.[32]
Coefficient of variation (CoV%) – This should be used over coherence to determine quality control, whenever available. CoV should be ≤10% in adults and ≤15% in children for two sets of R5.[32]
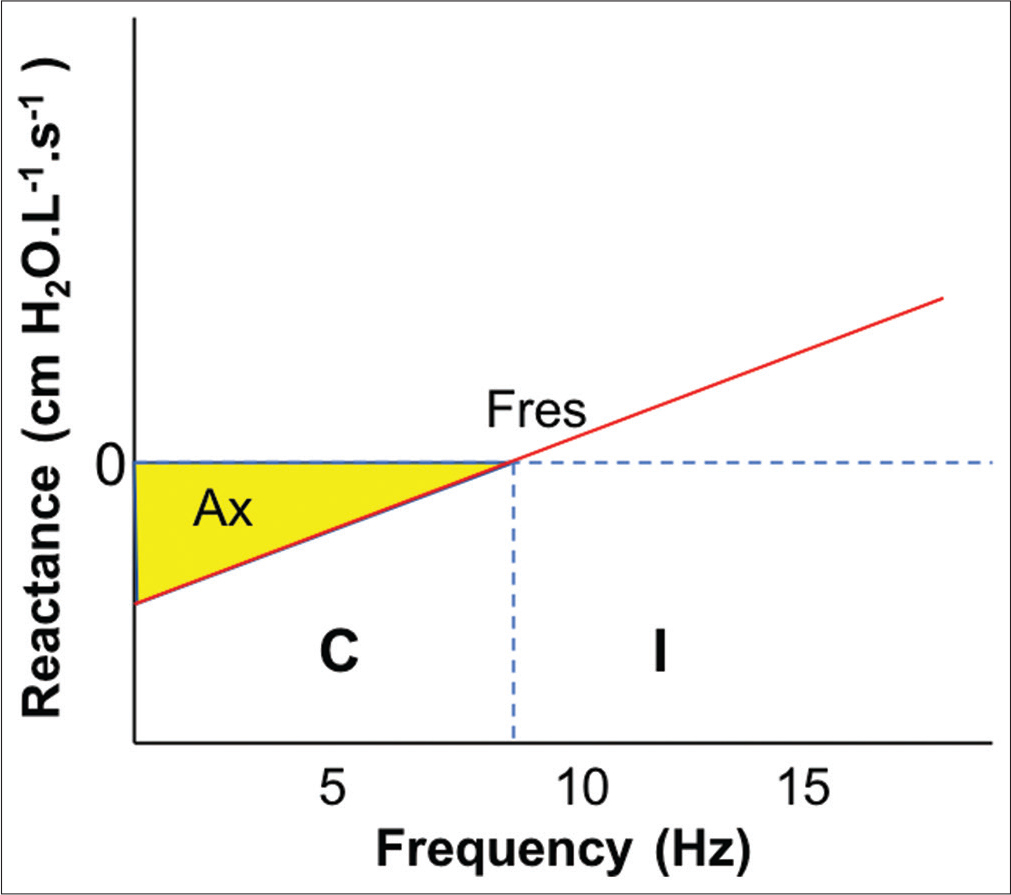
- Changes in reactance with frequency. Fres: Resonant frequency, Ax: Reactance area, C: Capacitance, I: Inertance.
TECHNIQUE
Calibration of the machine, at least once a day, is desired with the external resistor or as per the manufacturer’s specifications.[11] Bronchodilator medications (short-acting β-2 agonist for 4 h and long-acting β-2 agonist for 24 h) should be stopped before the procedure. After explaining the procedure (preferably by recorded video demonstration) to patient and attendants, anthropometric measurements (weight, height, and body mass index) are documented. Demographic (name, age, gender, area of residence, and identification number) and anthropometric parameters are entered in the machine after calibration. Patient is asked to sit on an examination stool/chair, with uncrossed legs to reduce the influence of extrathoracic pressure with straight back [Figure 4].[30] He/she is asked to hold the mouth piece with his/her teeth and to make a tight seal around it with lips to prevent any air leak during the FOT maneuver. A nose clip is applied to occlude both the nostrils and he/she is asked to breathe through mouth piece. Height of sitting stool/chair and/or mouth piece is adjusted to achieve a comfortable position for the patient with slight neck extension. As FOT is based on small pressure oscillations and a little change in resistance or air leak can affect the interpretations significantly, it is important to ensure adequate seal around nose and mouth piece. The cheeks, most compliant part of respiratory system in children, should be supported firmly either by patient him/herself or attendant to minimize wobbling [Figure 4].[20] After appropriate positioning, patient is asked to perform normal tidal breathing in a relaxed manner. An average of 10 respiratory efforts or 1 min, whichever is earlier, is required to assess the respiratory characteristics during any maneuver.[12] Acquisitions of minimum 30 s for adults and 16 s for children (<12 years of age) with at least three acceptable breaths are recommended.[32] Respiratory efforts meeting acceptability criteria [Table 1] are considered valid, whereas maneuvers with artifacts such as airflow obstruction by tongue or glottic closure, irregular breathing, coughing, crying, swallowing, and improper technique will be discarded by the machine. A maximum of three acceptable maneuvers are recorded and checked for coherence or CoV. Mean respiratory impedance (resistance and reactance), resonant frequency, and reactance area are documented. The procedure is repeated 15 min after inhaled short-acting β-2 agonist to identify any post-bronchodilator reversibility.
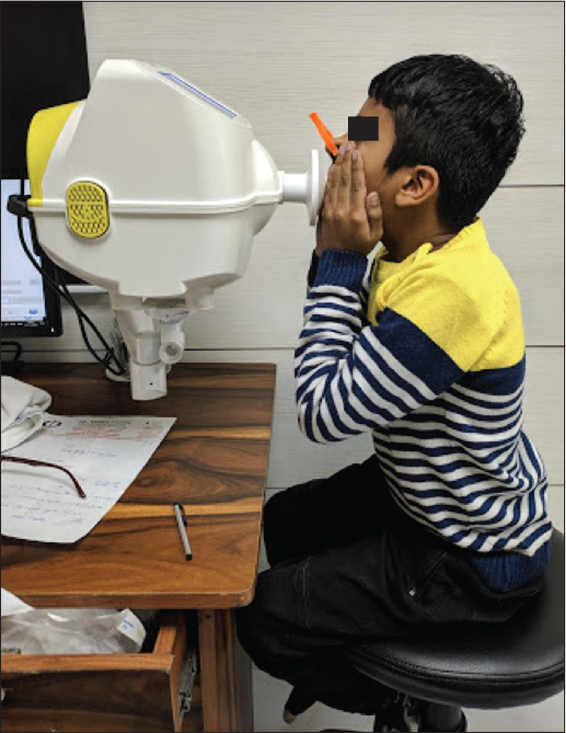
- Technique of performing oscillometry.
| Domain | Criterias |
|---|---|
| Patient position | Sitting position at comfortable height Back straight with slightly extended neck Legs uncrossed Nose clip on Cheek firmly supported |
| Patient-machine interface | Tight seal around mouth piece No artefact due to irregular breathing efforts, tongue obstruction, speaking or coughing during maneuver, glottis closure or swallowing |
NORMAL VALUES
-
Impedance – Several studies have provided reference values for respiratory characteristics till date.[20] The references might vary as per the ethnicity and the oscillation technique used in different machines.[26] The commonly used regression equations, by the machine, for calculating R and X based on height (H) in meters, weight (W) in kilograms, and age (A) in years are as follows:[33]
for men –
Rmen = –0.2454. H+0.001564. W–0.00055. A+0.5919
Xmen = 0.1479. H–0.000402. W–0.00022. A–0.1721 and for women –
Rwomen = –0.4300. H+0.00165. W–0.00070. A+0.9312
Xwomen = 0.2487. H–0.001700. W–0.00053. A–0.2158
Normative values from Indian populations need to be devised. Gupta et al. have recently demonstrated a negative correlation between oscillometry parameters with height followed by body mass index in Indian children, while evaluating airway reversibility in asthmatic patients.[16] There was no gender influence observed on any of the parameter.
Resonant frequency – The normal values of Fres varies in between 6 and 12 Hz in healthy adults[8,34] and it tends to be more in children
Reversibility – The recommended cutoffs for significant bronchodilator response in both adults and children are –40% in R5, +50% in X5, and –80% in Ax.[32] These values might vary with severity of disease and more studies are required before considering them as benchmark
Degree of bronchoconstriction – Cutoffs for X5 have varied from 50 to 80% and more studies are needed to provide reference values for specific populations.[32]
INTERPRETATION
Resistance (R) – Total, large/central, and small/ peripheral airway resistances are represented as R5, R19/20, and R5–R19/20. R5 is always higher than R19/20. This difference is practically negligible in adults, whereas it increases in younger children due to significant contribution by peripheral airway resistance. In peripheral airway obstruction, R5 will increase with normal R19/20 (and higher R5–R19/20) making frequency dependent airway resistance (R α 1/f).[24] In larger airway obstruction, both R5 and R19/20 will rise equally (with normal R5–R19/20), which will be frequency independent [Figure 5]. There will not be any change in restrictive lung diseases [Table 2]
Spiky pattern in inspiration, demonstrated by >2 standard deviation variation in subsequent efforts at 5 Hz, may suggest vocal cord dysfunction.[18] The finding needs to be supported with further research
Reactance (X) – It is usually measured at 5 Hz and becomes more negative in both peripheral airway obstruction and lung parenchymal disease [Figure 5]. It is not affected by large airway obstruction
Resonant frequency (Fres) – It increases (shift to right) in both restrictive and peripheral airway obstructive diseases.[24] It is not affected by large airway obstruction
Reactance area (Ax) – It increases in both small airway obstruction and restrictive diseases.[8] It is not affected by central airway problems.
| Conditions | R5 | R19/20 | R5– R19/20 | X5 | Ax | Fres |
|---|---|---|---|---|---|---|
| Peripheral obstruction | ↑↑↑ | N | ↑↑ | More negative | ↑↑ | ↑↑ |
| Central airway obstruction | ↑↑ | ↑↑ | N | N | N | N |
| Combined airway obstruction | ↑↑↑ | ↑↑ | ↑ | More negative | ↑↑ | ↑↑ |
| Restrictive lung disease | N | N | N | More negative | ↑↑ | ↑↑ |
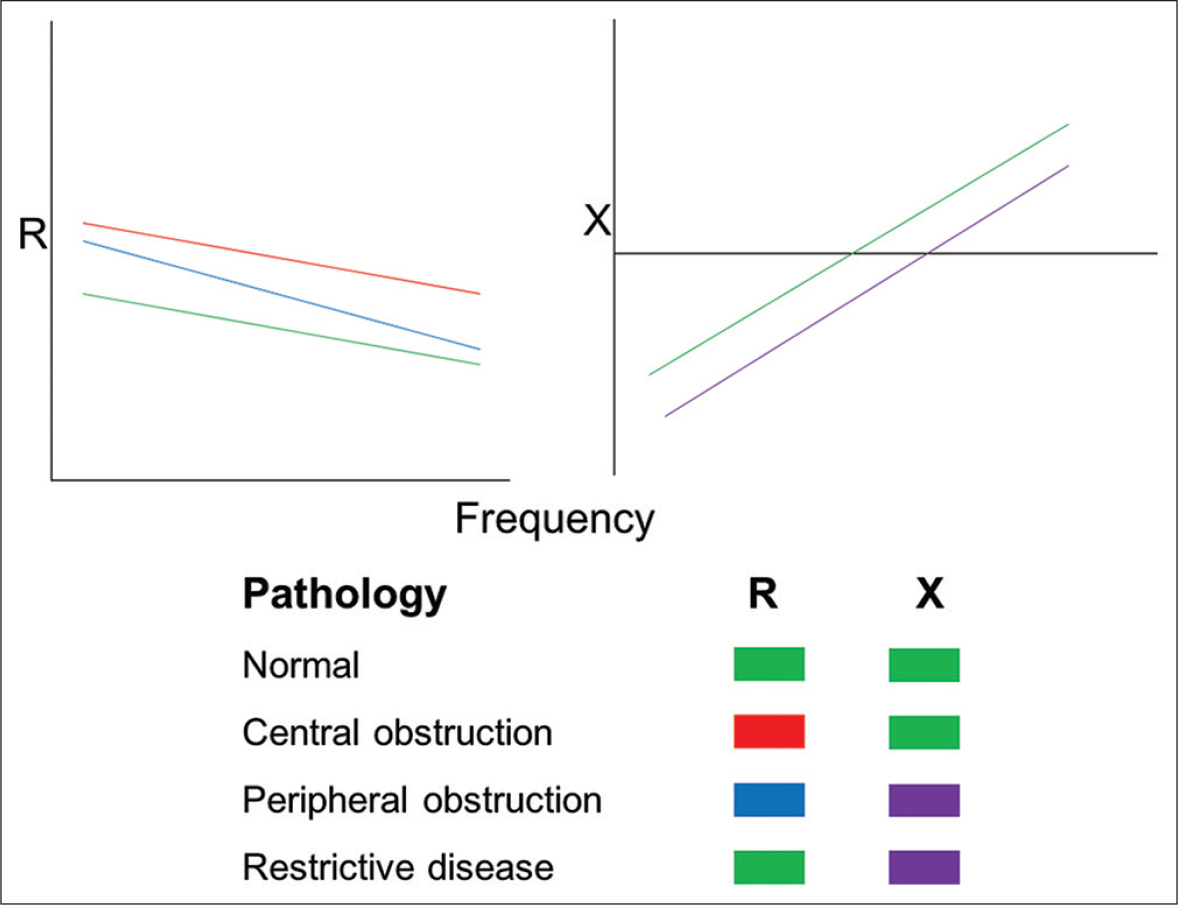
- Respiratory characteristics in health and disease. R – Resistance (in cm H2O.L-1.s-1), X – Reactance (in cm H2O.L-1.s-1). During normal healthy conditions, the resistance and reactance are at baseline (green). Various combinations of changes in these parameters will help in determining the nature and location of pathology.
COMPARISON WITH SPIROMETRY
Oscillometry is more sensitive for the detection of peripheral airway obstruction and restrictive diseases affecting lung parenchyma.[11,12] [Table 3] highlights the salient differences between spirometry and oscillometry.[8]
| Parameter | Spirometry | Oscillometry |
|---|---|---|
| Principle | Measures flow rates and lung volumes | Calculates impedance by measuring flow and pressure of sound waves |
| Parameters measured | FEV1, FVC, PEFR, FEF25-75% | Z, R, X, Fres, Ax |
| Type of breath required | Forced maneuver | Tidal breath |
| Patient cooperation needed | High | Minimal |
| Can be performed in children | >7 years | >2 years |
| Patients with neuromuscular weakness, intellectual disability, post cardiothoracic surgery | Procedure cannot be done | Can be done |
| Sensitivity for detection of peripheral airway obstruction | Low | High |
| Aerosol generation | High | Very low |
| Standardization of method | Yes | Yet to be done |
| References value | Available | Need more studies |
FEV1 – Forced Expiratory Volume in 1 second, FVC – Forced Vital Capacity, PEFR – Peak Expiratory Flow Rates, FEF25-75% - Forced Expiratory Flow at 25- 75% of FVC, Z – Impedance, R – Resistance, X – Reactance, Fres – Resonant frequency, Ax – Reactance area
Use of spirometry has been restricted in current COVID-19 pandemic due to reasons of enhanced risk of disease transmission by potential aerosol generation.[35] Forced breathing maneuver causes more aerosol generation due to “airway reopening phenomenon.”[36] Breathing till residual volume will reopen the collapsed alveoli causing increased air turbulence, leading to more production and release of smaller particles.[36] A small volume tidal breath, as used in oscillometry, will not cause much disturbance in the internal milieu and thus safeguarded in situations of active infections (such as influenza and corona). Gupta et al. have highlighted this concept recently, which suggest oscillometry procedure safer than spirometry in viral pandemic situations.[19]
CLINICAL APPLICATIONS OF OSCILLOMETRY
Provides practically useful information regarding the subtle changes in airways with greater sensitivity, in both children and adults, when compared to spirometry[37,38]
Useful to assess abnormal distal airway function, in case of clinical suspicion with normal spirometry[38,39]
Bronchodilator reversibility can be demonstrated with short-acting β-2 agonists and ipratropium[40,41]
Good potential in diagnosis and monitoring of restrictive lung diseases such as bronchopulmonary dysplasia,[42] cystic fibrosis,[43] and interstitial lung disease[44]
Feasible option in children, the elderly, and those with neuromuscular diseases and impaired intellect[24,26]
Potentially useful in patients on mechanical ventilation[45] and during sleep[11]
Safer than spirometry during viral pandemic situations (e.g., influenza and corona) due to less aerosol generation.[19] Oscillometry can be used to reliably diagnose and monitor patients with asthma and COVID-19 pneumonia.
[Figure 6] shows an algorithmic approach to a patient with oscillometric lung function assessment.
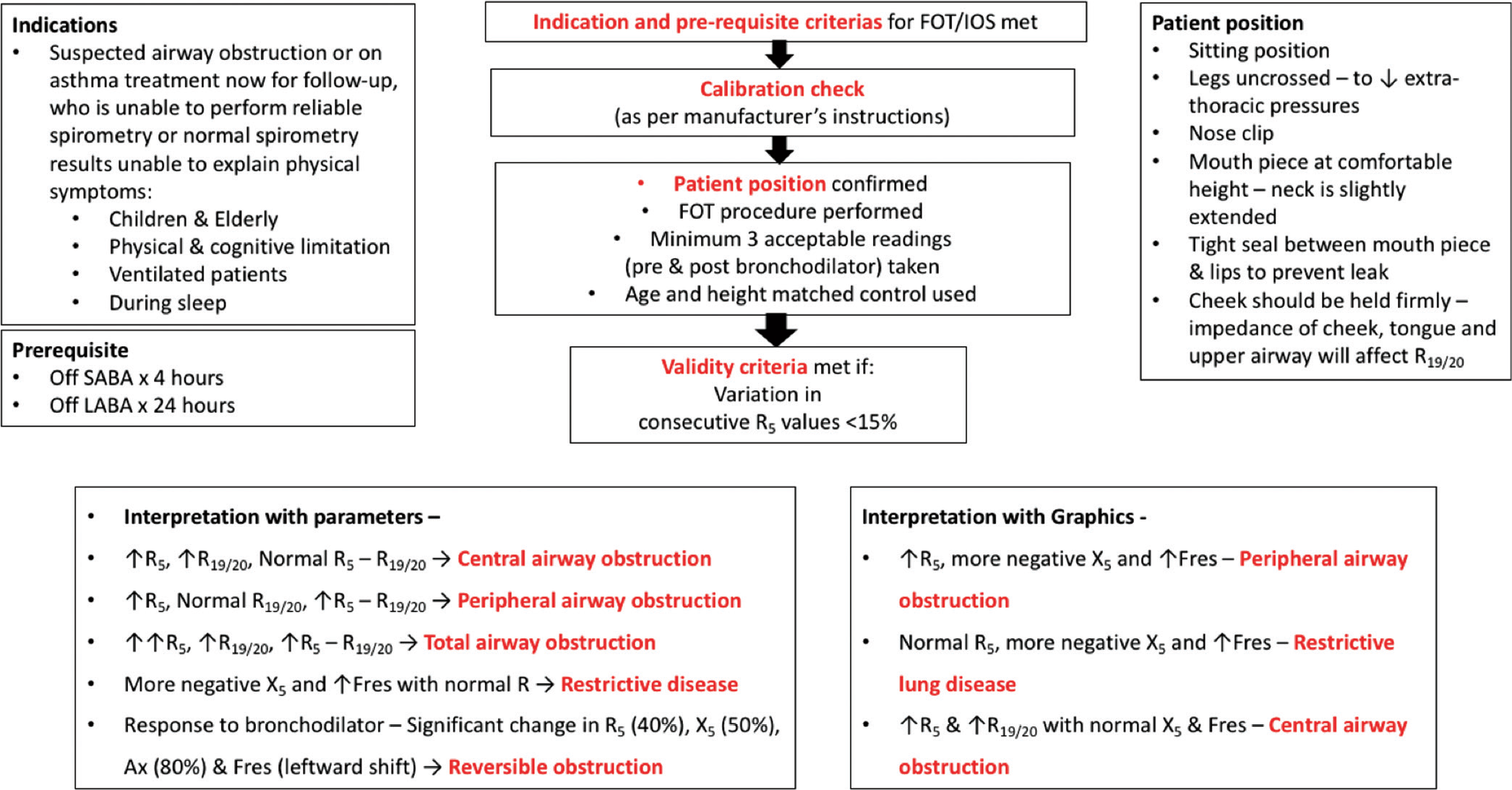
- Approach to a patient with oscillometric assessment. FOT: Forced oscillation technique, IOS: Impulse oscillometry, SABA: Short-acting β2 agonist, LABA: Long-acting β2 agonist, R: Resistance (in cm H2O.L-1.s-1), X: Reactance (in cm H2O.L-1.s-1), Fres: Resonant frequency (in Hz), Ax: Reactance area.
Limitations
Although this technique is tidal breath based, still a minimum amount of cooperation is needed from patients
Standardization of the available machines with different manufactures is needed
Reference values for different populations are not available
Reference cutoff values for bronchodilator reversibility need to be validated with more studies
Poor cheek support can reduce the resistance values[46]
More research required in restrictive diseases, ventilated, and/ or sedated patients and patients with vocal cord dysfunction.
CONCLUSION
Oscillometry, being a tidal breath-based technique, can be a real privilege to physicians and their patients for monitoring lung functions. It is more sensitive in detecting small airway pathologies than conventional spirometry. Limited aerosol generation could be another reason for its use in viral pandemics for monitoring lung functions. More research is required for identifying regional reference values and standardization of machines.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ J. 2014;7:12.
- [CrossRef] [PubMed] [Google Scholar]
- Spectrum of allergens and allergen biology in India. Int Arch Allergy Immunol. 2018;177:219-37.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge assessment among caregivers about various allergic disorders in a hospital-based pediatric outpatient department in North India. Indian J Allergy Asthma Immunol. 2020;34:112-6.
- [CrossRef] [Google Scholar]
- Prevalence of asthma-like symptoms in young children. Pediatr Pulmonol. 2007;42:723-8.
- [CrossRef] [PubMed] [Google Scholar]
- Global Strategy for Asthma Management and Prevention. 2020. Available from: http://www.ginasthma.org. [Last accessed on 2020 Oct 15]
- [Google Scholar]
- Approaches to asthma diagnosis in children and adults. Front Pediatr. 2019;7:148.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring lung function using sound waves: Role of the forced oscillation technique and impulse oscillometry system. Breathe (Sheff). 2015;11:57-65.
- [CrossRef] [PubMed] [Google Scholar]
- Self-reported physician practices for children with asthma: Are national guidelines followed? Pediatrics. 2000;106(Suppl 4):886-96.
- [Google Scholar]
- (Correcting) misdiagnosis of asthma: A cost effectiveness analysis. BMC Pulm Med. 2011;11:27.
- [CrossRef] [PubMed] [Google Scholar]
- An official American thoracic society/ European respiratory society statement: Pulmonary function testing in preschool children. Am J Respir Crit Care Med. 2007;175:1304-45.
- [CrossRef] [PubMed] [Google Scholar]
- Application of the forced oscillation technique in diagnosing and monitoring asthma in preschool children. Adv Respir Med. 2019;87:26-35.
- [Google Scholar]
- Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956;8:587-94.
- [CrossRef] [PubMed] [Google Scholar]
- The case for impulse oscillometry in the management of asthma in children and adults. Ann Allergy Asthma Immunol. 2017;118:664-71.
- [CrossRef] [PubMed] [Google Scholar]
- Impulse oscillometry: Reference values in children 100 to 150 cm in height and 3 to 10 years of age. Chest. 2005;128:1266-73.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of airway reversibility in asthmatic children using forced oscillation technique-a single-center experience from North India. Lung India 2020
- [CrossRef] [Google Scholar]
- Reference values of impulse oscillometric lung function indices in adults of advanced age. PLoS One. 2013;8:e63366.
- [CrossRef] [PubMed] [Google Scholar]
- Vocal cord dysfunction as demonstrated by impulse oscillometry. J Allergy Clin Immunol Pract. 2013;1:387-93.
- [CrossRef] [PubMed] [Google Scholar]
- Oscillometry-a reasonable option to monitor lung functions in the era of COVID-19 pandemic. Pediatr Pulmonol 2020
- [CrossRef] [PubMed] [Google Scholar]
- The forced oscillation technique in clinical practice: Methodology, recommendations and future developments. Eur Respir J. 2003;22:1026-41.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary mechanics by spectral analysis of forced random noise. J Clin Invest. 1975;56:1210-30.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical application of the forced oscillation technique. Intern Med. 2016;55:559-66.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of oscillometry devices using active mechanical test loads. ERJ Open Res. 2019;5:160-2019.
- [CrossRef] [PubMed] [Google Scholar]
- Impulse oscillometry: Interpretation and practical applications. Chest. 2014;146:841-7.
- [CrossRef] [PubMed] [Google Scholar]
- Oscillation mechanics of the respiratory system: Applications to lung disease. Crit Rev Biomed Eng. 2011;39:337-59.
- [CrossRef] [PubMed] [Google Scholar]
- Impulse oscillometry: The state-of-art for lung function testing. Lung India. 2016;33:410-6.
- [CrossRef] [PubMed] [Google Scholar]
- Oscillation mechanics of the respiratory system In: Macklem P, Mead J, eds. Handbook of Physiology, The Respiratory System, Mechanics of Breathing. Vol 3. Bethesda: American Physiological Society; 1986. p. :145-66.
- [Google Scholar]
- Changes of respiratory input impedance during breathing in humans. J Appl Physiol. 1992;73:2355-62.
- [CrossRef] [PubMed] [Google Scholar]
- Forced Oscillation Technique and Impulse Oscillometry. Lung Function Testing: European Respiratory Society Monograph 2005:72-105.
- [CrossRef] [Google Scholar]
- Impulse oscillometry in the evaluation of diseases of the airways in children. Ann Allergy Asthma Immunol. 2011;106:191-9.
- [CrossRef] [PubMed] [Google Scholar]
- Impulse oscillometry provides an effective measure of lung dysfunction in 4-year-old children at risk for persistent asthma. J Allergy Clin Immunol. 2003;112:317-22.
- [CrossRef] [PubMed] [Google Scholar]
- Technical standards for respiratory oscillometry. Eur Respir J. 2020;55:1900753.
- [CrossRef] [PubMed] [Google Scholar]
- Total respiratory impedance measured by means of the forced oscillation technique in subjects with and without respiratory complaints. Eur Respir J. 1996;9:131-9.
- [CrossRef] [PubMed] [Google Scholar]
- Contribution of impedance measurement of the respiratory system to bronchial challenge tests. J Asthma. 1988;25:259-67.
- [CrossRef] [PubMed] [Google Scholar]
- Spirometry in COVID-19 times-an emerging dilemma. Indian Pediatr. 2020;57:779-80.
- [CrossRef] [PubMed] [Google Scholar]
- A study of the use of impulse oscillometry in the evaluation of children with asthma: Analysis of lung parameters, order effect, and utility compared with spirometry. Pediatr Pulmonol. 2012;47:18-26.
- [CrossRef] [PubMed] [Google Scholar]
- Distal airway function in symptomatic subjects with normal spirometry following world trade center dust exposure. Chest. 2007;132:1275-82.
- [CrossRef] [PubMed] [Google Scholar]
- Small airway dysfunction by impulse oscillometry in asthmatic patients with normal forced expiratory volume in the 1st second values. Allergy Asthma Proc. 2013;34:e14-20.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of asthma and wheezing in the first 6 years of life: Follow-up through adolescence. Am J Respir Crit Care Med. 2005;172:1253-8.
- [CrossRef] [PubMed] [Google Scholar]
- Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948-68.
- [CrossRef] [PubMed] [Google Scholar]
- Lung function and bronchial responsiveness measured by forced oscillometry after bronchopulmonary dysplasia. Arch Dis Child. 1988;63:727-32.
- [CrossRef] [PubMed] [Google Scholar]
- Lung function distinguishes preschool children with CF from healthy controls in a multi-center setting. Pediatr Pulmonol. 2012;47:597-605.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of inspiratory and expiratory reactance in interstitial lung disease. Respir Med. 2013;107:875-82.
- [CrossRef] [PubMed] [Google Scholar]
- Oscillatory resistance measured during noninvasive proportional assist ventilation. Am J Respir Crit Care Med. 2001;164:790-4.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of cheek support on respiratory impedance measured by forced oscillation technique. Springerplus. 2013;2:342.
- [CrossRef] [PubMed] [Google Scholar]






