Translate this page into:
Polycystic ovarian syndrome in adolescence
*Corresponding author: Preeti Manmohan Galagali, Consultant Adolescent Health Specialist and Director, Bengaluru Adolescent Care and Counselling Centre, 528 2nd Block Rajajinagar, Bengaluru - 560 079, Karnataka, India. drpgalagali@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Galagali PM. Polycystic ovarian syndrome in adolescence. Karnataka Paediatr J 2020;35(2):95-9.
Abstract
Polycystic ovarian syndrome (PCOS) may clinically manifest for the 1st time in adolescence. Hyperandrogenemia and oligo-anovulation are the two essential criteria for the diagnosis of PCOS. PCOS has long-term effects on cardiovascular, endocrinal, reproductive, and metabolic health. Early management of PCOS mitigates its long-term effects on health. Therapeutic lifestyle management and psychological counseling form the main stay of treatment in adolescence. Diagnosis of PCOS in adolescence is revisited and confirmed in adulthood. Management of PCOS is multidisciplinary and requires long-term regular follow-up in adolescence and adulthood.
Keywords
Polycystic ovarian syndrome
Adolescence
Hyperandrogenemia
Oligo-anovulation
INTRODUCTION
Polycystic ovarian syndrome (PCOS) is the most common female endocrinopathy. Clinical features of PCOS are usually evident in adolescence. Management in adolescence can mitigate the long-term effects of PCOS.
DIAGNOSIS OF PCOS IN ADOLESCENCE
It is difficult to make an accurate diagnosis of PCOS in the adolescent period using the conventional adult Rotterdam criteria that include the presence of two of the following: Oligoanovulation, hyperandrogenism, and polycystic ovaries on ultrasound. All the three features are a part of normal growth and development in adolescence. Oligo-anovulation characterized by irregular periods is normal in the 1st few years after attaining menarche. About 80% of adolescents have acne. Severe acne that is resistant to treatment is a clinical indicator of hyperandrogenism. Multiple cysts in the ovaries are commonly seen on ultrasound in adolescence. An ovarian volume >12 cc in adolescence is considered by some researchers as a pointer toward PCOS.
The recently published International Guidelines state that both oligo-anovulation and hyperandrogenism should be present for diagnosing adolescent PCOS and polycystic ovaries on ultrasound are not considered as a diagnostic criterion.[1] Other causes of hyperandrogenism and anovulation have to be excluded before making a diagnosis of PCOS. These include congenital adrenal hyperplasia, androgen secreting tumors, Cushing’s syndrome, thyroid dysfunction, and hyperprolactinemia.
Ovulatory dysfunction clinically presents as irregular menstrual cycles. Oligo-anovulation in adolescents is defined according to the gynecological age (number of years after attaining menarche).
For adolescents who are 1–<3 years post-menarche, the interval between menstrual cycles <21 days or >45 days is considered oligo-anovulation.
For adolescents who are 3 years post-menarche, the interval between menstrual cycles <21 or >35 days or <8 cycles/year is considered oligo-anovulation.
For adolescents 1 year post-menarche, duration of >90 days for any one cycle and if menarche is not attained by the age of 15 years or >3 years post-thelarche, it is considered oligo-anovulation.
Clinical diagnostic criteria for hyperandrogenism include severe acne and hirsutism in adolescence, as shown in [Figure 1]. Biochemical criteria of hyperandrogenism are increased calculated free testosterone and free androgen index. In adolescence, normal levels of testosterone are not well defined; hence, persistent testosterone elevation above adult norms is a reliable reference for hyperandrogenism. Longitudinal follow-up of suspected cases of PCOS in adolescence is recommended and the diagnosis is revisited at 8 years post-menarche.

- A 14-year-old girl with acne, hirsutism, and acanthosis nigricans suggestive of polycystic ovarian syndrome.
PATHOPHYSIOLOGY
Pathophysiology of PCOS is not clearly delineated. Both genetic and environmental factors contribute to its development.[2,3] Inheritance is said to be both X linked and autosomal dominant. In most cases, there is a family clustering in female siblings and a positive family history of diabetes. The following postulates have been put forth for the development of PCOS:
A defect in the insulin receptor gene has been demonstrated in few patients with PCOS, leading to insulin resistance and hyperinsulinemia. Hyperinsulinemia results in hyperandrogenemia and dyslipidemia.
PCOS is said to be due to disordered hypersensitivity of pituitary to the secretion of gonadotropin-releasing hormone (GnRH). This results in increase in secretion of both luteinizing hormone and androgens from ovaries. This causes oligo-anovulation and hyperandrogenism. Androgens are converted to estrogens that further augment pituitary hypersensitivity to GnRH.
Obesity is associated with PCOS as it leads to insulin resistance and hyperinsulinemia.
Adverse intrauterine environment due to maternal undernutrition or anemia may result in neuroendocrine dysregulation in the fetus leading to insulin resistance and intrauterine growth restriction (IUGR) babies. IUGR babies may develop features of PCOS in adolescence, especially if they have rapid weight gain in infancy and childhood. Rapid weight gain exacerbates the existing hyperinsulinemic metabolic state in these children.
LONG-TERM EFFECTS OF PCOS
PCOS can lead to both morbidity and mortality over the life span, as shown in [Figure 2].[3,4] Health professionals should manage adolescents with signs and symptoms of PCOS early in life. The long-term effects of PCOS are the following:
Cardiovascular problems: Hypertension, coronary artery disease, hyperlipidemia, and obstructive sleep apnea syndrome are seen in patients with PCOS.
Endocrinal problems: Type 2 diabetes, non-alcoholic fatty liver disease, and metabolic syndrome may develop in adolescence or adulthood. Metabolic syndrome comprises cardiovascular disease risk factors associated with insulin resistance, namely, glucose intolerance, dyslipidemia, hypertension, and central obesity. Hyperandrogenemia in PCOS may contribute to metabolic syndrome independent of obesity. Hence, lean PCOS is also prone to develop metabolic syndrome.
Reproductive health problems: Infertility, gestational diabetes, pre-eclamptic toxemia, preterm labor, recurrent miscarriage, and endometrial carcinoma are said to occur with adult PCOS. PCOS contributes to 30–40% of overall infertility in women. Unopposed estrogenic stimulation in PCOS leads to endometrial carcinoma in adulthood.
Psychosocial issues: Body image problems, depression, anxiety, suicidal behavior, eating disorders, disordered eating, and poor self-esteem are associated with PCOS.
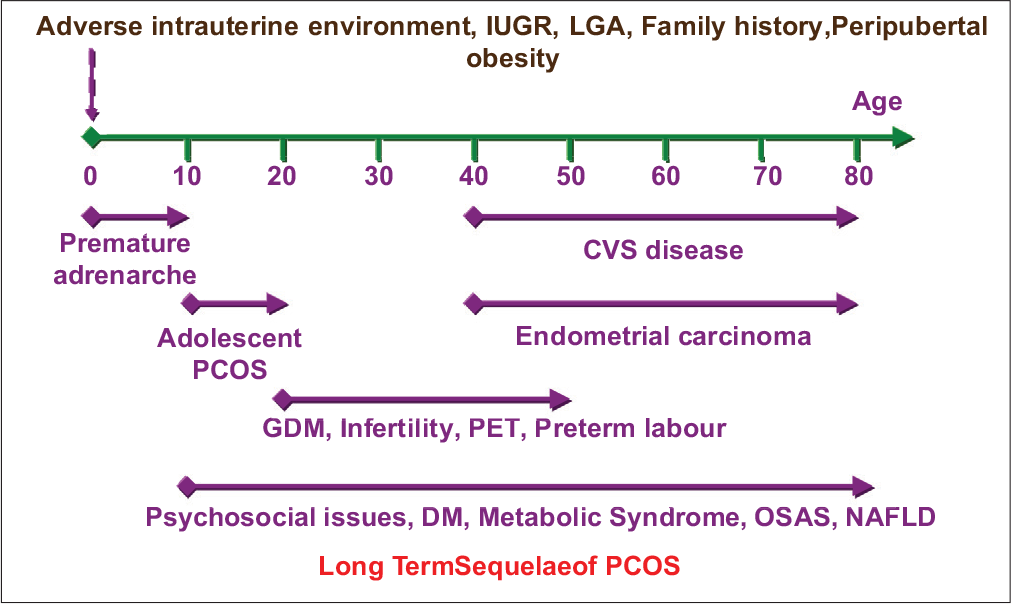
- Long-term sequelae of polycystic ovarian syndrome. CVS: Cardiovascular, GDM: Gestational diabetes mellitus, PET: Preeclamptic toxemia, DM: Diabetes mellitus, OSAS: Obstructive sleep apnea syndrome, NAFLD: Non-alcoholic fatty liver disease.
Clinical presentation
Menstrual disorders with hirsutism are the most common clinical presentation of PCOS in adolescence.[2-4] Adolescents may present with secondary or primary amenorrhea. Obesity is seen in 50–70% of adolescents with PCOS. They have severe acne that is refractory to topical treatment and have androgenic alopecia in the form of male pattern frontal balding. They usually have body image concerns and may have clinical depression and anxiety. PCOS can also present with primary amenorrhea in adolescence.
The clinician should be sensitive and empathetic during history taking and examination. HEEADSSS psychosocial history should be taken from the adolescent in privacy and with confidentiality. HEEADSSS is an acronym that stands for various domains of an adolescent’s life including home, eating, education, activities, drugs, suicide/depression, sexuality, and safety. Dietary intake, level of physical activity, details of media usage, body image concerns, bullying and teasing by peers, difficulty in sleep, snoring, and features of depression and anxiety should be elicited. Eating disorders and disordered eating may coexist with PCOS and should be asked for in particular. Menstrual history should be taken in detail. Family history of similar complaints and a birth history regarding IUGR should also be taken by the clinician.
On examination, height, weight, and body mass index (BMI) are plotted on the Indian Academy of Pediatrics growth charts.[5] It is also important to measure waist circumference (for evaluating central adiposity), sexual maturity rating, and blood pressure.[6] The BMI cutoffs for overweight and obesity are lower in South Asians as they are prone to develop metabolic syndrome at lower values. BMI >25 signifies obesity and between 23 and 25 indicates overweight. Waist circumference varies with age and centile charts are available. At 18 years of age and above, waist circumference of >80 cm indicates central adiposity. Hypertension is often associated with PCOS, obesity, and metabolic syndrome.
Hirsutism is graded using the modified Ferriman–Gallwey scoring system and acne is graded as mild, moderate, or severe. A modified Ferriman–Gallwey score of >4–6, depending on ethnicity is considered significant. These scoring systems assess clinical severity and help in follow-up. They give objective assessment of improvement when the adolescent is on treatment. Acanthosis nigricans, a clinical indicator of insulin resistance, may also be seen, as shown in [Figure 1]. Androgenic alopecia, clitoromegaly, increased muscle mass, and deepening of voice usually indicate an androgen-producing tumor. A mental health assessment for depression, anxiety, eating disorders, and suicidal behavior including ideation and thoughts is also conducted.
Investigations are done to demonstrate biochemical hyperandrogenemia and to rule out other causes of hyperandrogenemia and amenorrhea.[2-4,7] These include calculated free testosterone, calculated total bioavailable testosterone, free androgen index. 17-hydroxyprogesterone (to rule out congenital adrenal hyperplasia), dehydroepiandrosterone (to rule out adrenal tumor), cortisol, thyroid function tests, prolactin, urine pregnancy test, and ultrasound (to rule out adrenal and ovarian tumors) are advised.
It is recommended to use liquid chromatography–mass spectrometry and extraction/chromatography immunoassay for the accurate assessment of total or free testosterone. Enzyme-linked radioimmunoassays for testosterone should not be used preferably as they lack accuracy. High levels of testosterone have not been clearly defined in adolescence and a level above 55 ng/dl may be considered elevated. If the adolescent is on oral contraceptives, it is recommended to stop these drugs for 3 months before a testosterone assessment as these are known to interfere with the biochemical result.
If clinical features of insulin resistance and metabolic syndrome are present, namely, acanthosis nigricans, overweight and hypertension, an oral glucose tolerance test, HBA1c, lipid profile, and liver function tests are mandatory. These are also indicated if there is a family history of PCOS, diabetes mellitus, and an early cardiovascular event at <55 years in a close relative.
Management
Children who were born as IUGR, large for gestational age, and whose mothers have PCOS are known to develop PCOS in adolescence. Those who put on weight rapidly in peripubertal years and with premature adrenarche are at risk. Hence, health professionals should closely follow-up these children with annual health checkups and ensure optimal weight at all ages. They should impart anticipatory guidance regarding balanced nutrition, physical activity, and healthy media usage.
Management of adolescent PCOS is multidisciplinary. Pediatrician, gynecologist, endocrinologist, nutritionist, dermatologist, and psychologists should collaborate for optimizing the case management. Goals of treatment include immediate relief of symptoms and prevention of long-term sequelae.[7]
Therapeutic lifestyle change (TLC) and psychosocial support with culture sensitive, respectful, and empathetic counseling are the cornerstones of therapy. Technique of motivational interviewing should be used by health professionals to encourage adolescents to eat a balanced wholesome diet and to increase physical activity. Intake of equal amount of carbohydrates and protein is encouraged along with food rich in omega 3 fatty acids such as fish, germinated sprouts, and walnuts. Adolescents with obesity and metabolic syndrome should have food with low glycemic index like whole grains and fiber. They should avoid intake of transfats in the form of processed food, bakery products, and fried food. Weight-related stigmatization is to be avoided during counseling. Behavioral modification for weight reduction includes goal setting, self and stimulus control (to avoid intake of high fat salt and sugar diet), mindful and slow eating, and assertive training to deal with negative peer pressure. Under the influence of peers, adolescents are known to binge on high calorie nutrient poor snacks.
Adolescents are counseled regarding benefits of regular moderate-to-severe intensity aerobic exercise for a minimum of 60 min/day and muscle and bone strengthening exercise at least 3 days in a week. Fun activities such as cycling, outdoor group play, tennis, badminton, and swimming are encouraged. Sedentary activities like digital media viewing are limited to 30–60 min/day. Parents are motivated to formulate a family media plan and role model a healthy lifestyle. Weight reduction of even 5% is known to result in spontaneous resumption of menstrual cycles and lower androgen levels.
Life skills such as stress management, relaxation techniques (yoga, meditation, and hobbies) problem solving, coping skills, and critical thinking are taught to adolescents to prevent emotional eating and to deal with body image issues. Depression, anxiety, and eating disorders are managed by cognitive behavior therapy and interpersonal therapy. Moderate-to-severe cases of depression and anxiety may require a psychiatric referral and a prescription of selective serotonin reuptake inhibitors like fluoxetine in a dose of 10–40 mg OD for 9–12 months.
Pharmacotherapy of PCOS includes drugs for the management of metabolic syndrome, Type 2 diabetes mellitus, menstrual irregularities, hirsutism, and acne. Metformin can be used if there is evidence of overweight, metabolic syndrome, Type 2 diabetes mellitus, and insulin resistance. The initial dose is 500 mg OD and can be increased to 1000 mg in daily divided doses. Side effects of metformin are nausea, vomiting, and dyspepsia.
Combination oral contraceptives (COC) containing ethinyl estradiol (at lowest effective dose 20–30 μg) and desogestrel are used for 6–12 cycles to regularize menstrual cycles, to decrease hirsutism, and to prevent the development of endometrial carcinoma. COC can cause thromboembolic phenomena and their use is restricted in adolescents with hyperlipidemia and hypertension. Cyclical progesterone in the form of medroxyprogesterone acetate 10 mg OD is an alternative to COC in adolescents who do not have hirsutism.
Antiandrogens like spironolactone 50–100 mg BD may be used for the management of hirsutism. Minocycline 50 mg OD is used for the treatment of severe acne. It may require therapy with retinoic acid compounds under the supervision of a dermatologist. Cosmetic procedures such as epilation, bleaching, waxing, chemical depilatory creams, electrolysis, laser, and eflornithine hydrochloride cream could also be used for managing hirsutism.
Clomiphene citrate, gonadotropins, laparoscopic surgery, and in vitro fertilization may be considered in married adolescents with PCOS and infertility. Bariatric surgery is recommended for morbidly obese adolescents with BMI > 35, with metabolic complications, after they have attained Tanner Stage 5 and have had a poor response to therapeutic lifestyle change and pharmacotherapy for 6–12 months.
Regular follow-up of adolescent PCOS is essential to mitigate immediate health problems and long-term sequelae. Frequent health visits at 1–2 months interval are recommended until menstrual regularity and emotional well-being are attained. Annual health checkups until adulthood are essential. The diagnosis is revisited after 8 years of menarche and a transition of care from the pediatrician to the adult physician is carefully planned.[1] Women with a confirmed diagnosis of PCOS would require regular health checkups and screening for cardiovascular issues, metabolic problems, and endometrial cancer over the entire life span.
CONCLUSION
Oligoanovulation and features suggestive of hyperandrogenemia in adolescence are pointers towards PCOS. It can lead to body image issues, mental disorders and metabolic syndrome in adolescence. Management of PCOS in adolescence is known to reduce its long term complications of cardiovascular disease, infertility and endometrial carcinoma in adulthood. Long term follow up of patients with PCOS is recommended over the entire life span.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018;110:364-79.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis of polycystic ovary syndrome during adolescence. Horm Res Paediatr. 2015;83:376-89.
- [CrossRef] [PubMed] [Google Scholar]
- Polycystic ovary syndrome in adolescence: Diagnostic and therapeutic strategies. Transl Pediatr. 2017;6:248-55.
- [CrossRef] [PubMed] [Google Scholar]
- Revised IAP growth charts for height, weight and body mass index for 5-to 18-year-old Indian children. Indian Pediatr. 2015;52:47-55.
- [CrossRef] [PubMed] [Google Scholar]
- Waist circumference percentiles in 2-18 year old Indian children. J Pediatr. 2014;164:1358-62.
- [CrossRef] [PubMed] [Google Scholar]
- Polycystic ovarian syndrome in adolescents In: Galagali P, ed. Suicide Prevention and Intervention Module. Indian: Indian Academy of Pediatrics for the Members; 2018. p. :79-83.
- [Google Scholar]






