Translate this page into:
Neonatal intubation: Can we make it better? A journey from ideation to intellectual property rights
*Corresponding author: Srinivasa Murthy Doreswamy, Department of Pediatrics, JSS Academy of Higher Education and Research, Mysuru, Karnataka, India. drdsrinivasa@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Doreswamy SM. Neonatal intubation: Can we make it better? A journey from ideation to intellectual property rights. Karnataka Paediatr J 2021;36(2):101-5.
Abstract
Objectives:
Neonatal intubation is regarded as one of the elite skills a medical professional; particularly a pediatrician could aspire to master. More the practice, the skill gets refined so that the success rate improves. However, it is not uncommon even for most experienced professional to fail in an intubation attempt. Why does it happen? Is there a solution? This article discusses the journey from ideation to intellectual property rights.
Materials and Methods:
Observational study followed by Randomised control study.
Results:
Reduction in the pressure exerted on upper jaw during intubation from 455 to 80 KPa and decrease in blocked visual area from 38.5 to 12%.
Conclusion:
Appropriate design modification of neonatal laryngoscope is potentially more safe and easy to use.
Keywords
Neonatal intubation
NOBL scope
Innovation
INTRODUCTION
Neonatal intubation is regarded as one of the elite skills a medical professional; particularly a pediatrician could aspire to master. More the practice, the skill gets refined so that the success rate improves.[1] However, it is not uncommon even for most experienced professional to fail in an intubation attempt. Why does it happen? Is there a solution?
Many of the intubation attempts result in trauma to the upper jaw of the neonates. Unfortunately, these are rarely documented and reported in any scientific platform.[2,3] How big is this trauma? Can this be avoided?
Problem statement
It is often difficult to intubate neonates particularly if they are tiny premature babies. We can look at this problem in two different ways.
The most common approach would be to accept the limitation of individual’s skill, given the difficult anatomy they have to deal with. This approach leads to elimination of any opportunity to find a solution.
The second and an unusual approach would be to deny the limitation of individual’s skill and explore the limitation of other associated factors involved in neonatal intubation. The second approach is unfortunately non-intuitive and remains unexplored in a niche. This article is the narration of how the second approach was successful in finding a solution for the stated problem.
History of neonatal laryngoscope
1878 – William MacEwan attempted adult intubation using his finger as guide. A direct laryngoscope was developed by Alfred Kirstein in 1895 which improved the technique of adult intubation compared to finger guided approach. It was in 1914 McGill developed Speculum laryngoscope which is the forerunner of modern laryngoscope. As the pediatric care improved, the McGill blade was modified in its size to suit children by 1940. A curved speculum blade was introduced for children by Macintosh in 1943. Significant change in the design of laryngoscope keeping in mind small infants was done by Miller in 1946 by introducing a straight blade. All these modifications hinged on changing either the size or the curvature of the blade without substantially altering its design.[4] The smaller ones are used in neonatal practice.
MATERIALS AND METHODS
Ideation
Neonatal intubation is difficult primarily because the neonatal airway anatomy considerably differs from that of adults and older children. There was no laryngoscope specifically designed for use in neonates. This formed the seed for ideation.
Ideation primarily is a creative mental process of developing a thought pattern and a plan sequence to solve a problem. Ideation is not just limited to formation of an idea but also act on it further until proof of concept is demonstrated.
Designing a new laryngoscope exclusively for neonates started with the study of the mismatch between the neonatal airway anatomy and the design of the laryngoscope in use. On studying the mismatch, two important design flaws became evident [Figure 1].

- Design flaws associated with conventional pediatric laryngoscope.
The size of the blade-Hinge complex was too big resulting in blocking the vision of the operator
The lateral flange on the intraoral portion of the blade, which is designed to restrain tongue on to a side during intubation in adults, is not useful in neonates. Added to this, the space available for intubation substantially decreases and also result in traumatizing the alveolar margin of the upper jaw.
Path ahead
As there was no scientific literature substantiating the above findings, a robust study had to be designed, conducted, and published to educate the scientific community. Following this, a new laryngoscope had to be designed which essentially eliminated the two design flaws noted.
Background study
A study was designed and conducted to measure the inadvertent force exerted on the upper jaw of the neonate (Mannikin) during intubation.[5] A pressure sensitive film was taped to the upper jaw of the Mannikin and the volunteers were requested to intubate. The force applied on the upper jaw resulted in the color change in the film which could be quantified using the graph provided by the manufacturer. Thirty volunteers with various levels of experience in neonatal care participated in the study and a total of 90 attempts were analyzed.
RESULTS 1
Overall pressure applied (Mean [SD]) over the upper jaw was 568 (78) Kilo pascals. This was more than twice the pressure that is shown to cause permanent tissue injury in animal models (around 250 KPa). There was no significant difference between the pressure exerted by frequent intubators (>6 intubation in a year) and less frequent intubators (<6 intubations per year).
In the same study, we also noted that 48% of the area of mouth was occupied by the laryngoscope hinge which blocked the vision (data unpublished).
Several take away message form this study was:
Our observation of lateral flange traumatizing the upper jaw was true and significant
This was prevalent among all experience categories of health-care professionals
Higher experience in neonatal intubation did not eliminate this harm
Nearly half of the area (Mouth) was blocked by the hinge of the laryngoscope blade which decreased both the area of operation and vision.
Overall, we could conclude that there is lot to do with the design of laryngoscope than the individual expertise.
NOBL scope
Neonatal offset blade laryngoscope for potentially safe intubation in neonates.
Design of the NOBL scope
Initial study bolstered the argument of laryngoscope design being one of the main contributors for difficulty in neonatal intubation and hence fixing that was an important step forward.
The new design obviously focused on eliminating the bulky hinge of the laryngoscope blade and the lateral flange. This necessitated that the blade to nearly float in the oral cavity by anchoring it at a distant point. After couple of designs and re designs, a blade which was offset from the handle was designed. [Figure 2] shows the illustration and a 3 D printed non-functional model of NOBL scope.
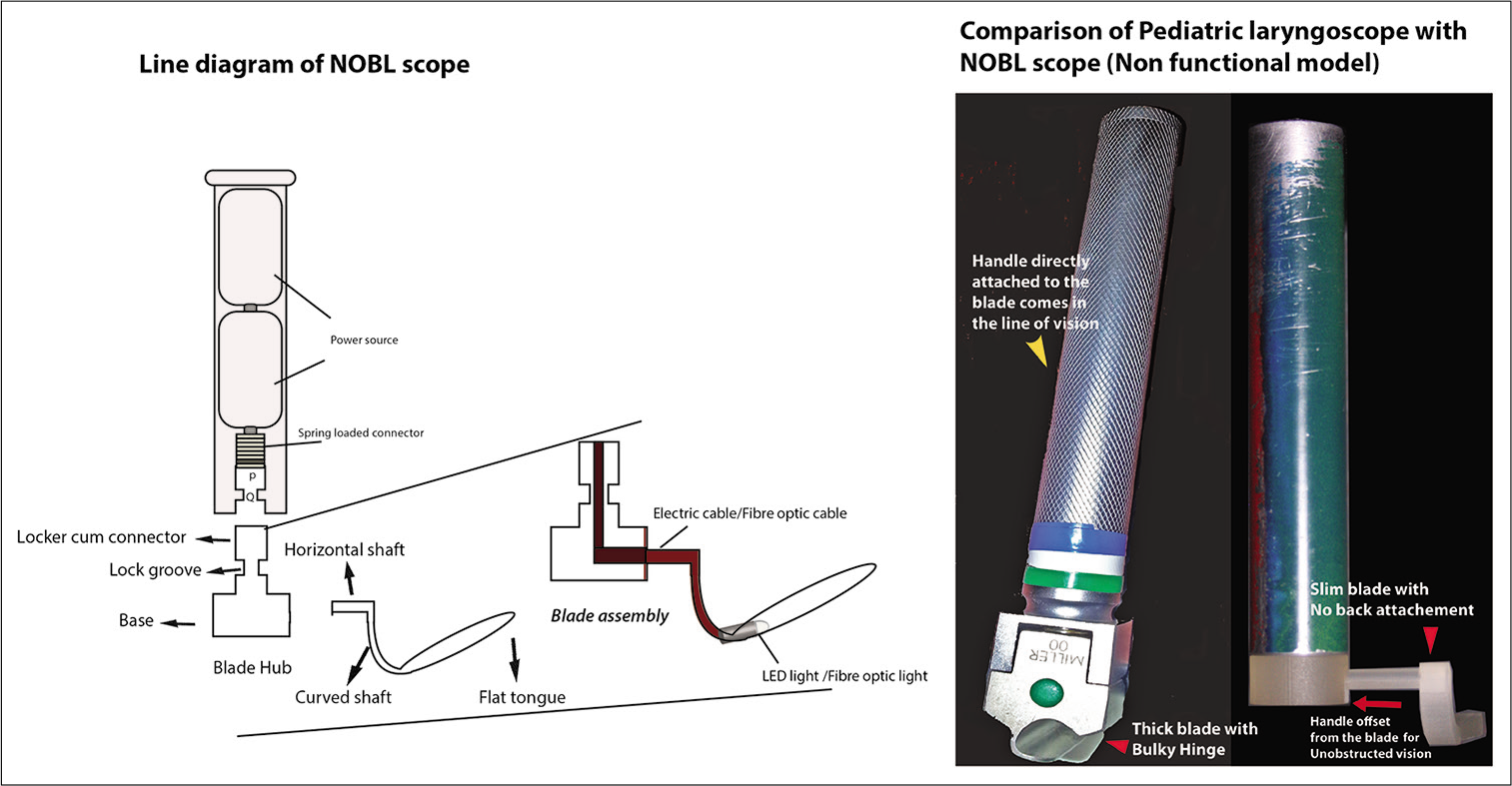
- NOBL Scope – Illustration and comparison with conventional laryngoscope.
Description
The new laryngoscope [Figure 3] has a novel design featuring the handle being offset from the blade by a horizontal element. The thick bulky hinge lock is eliminated from the line of vision to enhance the visibility of the larynx.
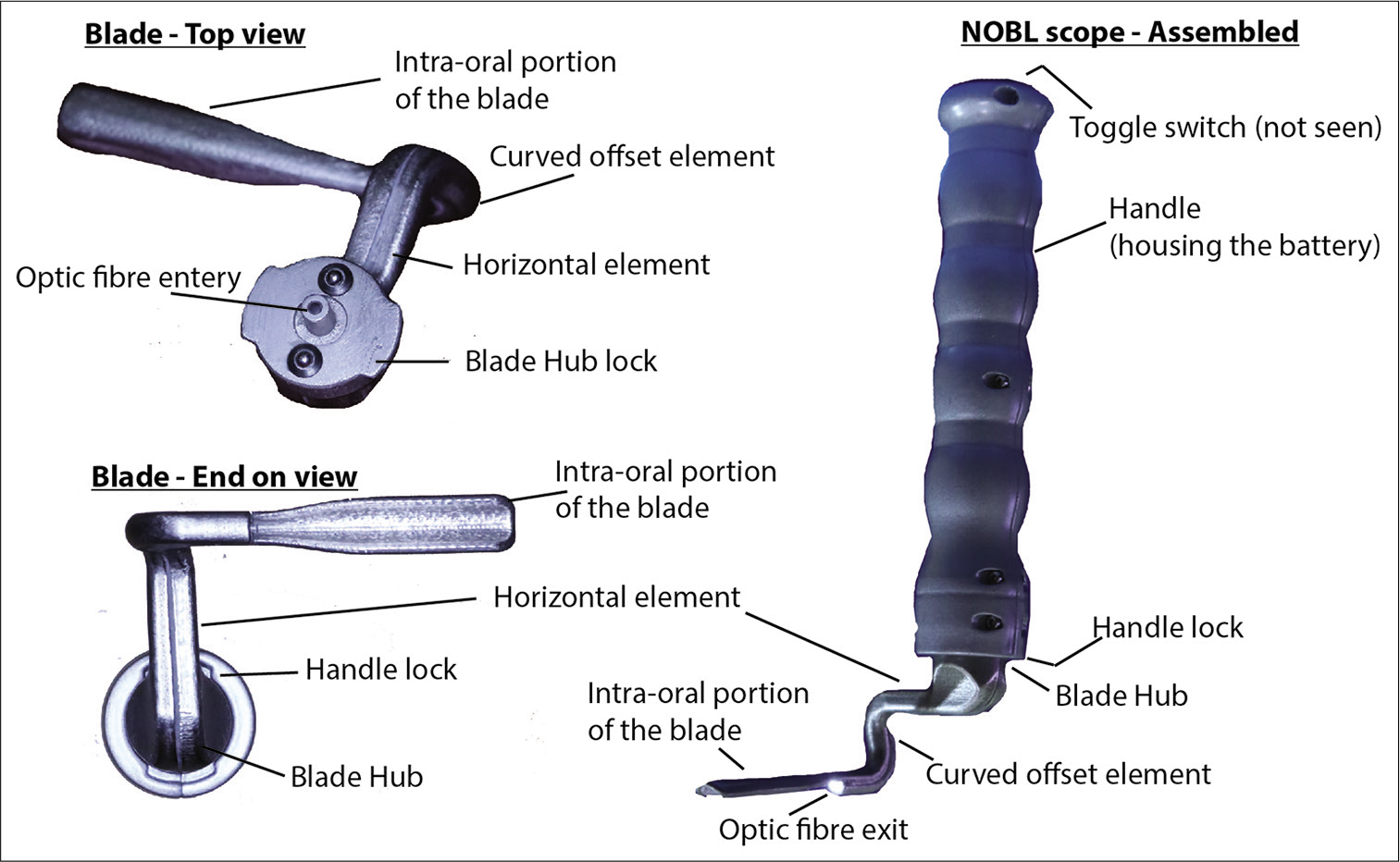
- Functional NOBL scope – parts.
The new device has a handle which houses battery, toggle switch and a LED light source. The handle has a specifically designed locking system for the blade which actuates when the blade is aligned and turned in anticlockwise direction.
The blade has a small hub which serves as the handle lock. The hub is separated from the intraoral portion of the blade by a horizontal element which anatomically curves at 90 degrees twice and leads to the handle. The hub and the offset element have an optical fiber running inside its center. The tip of the optic fiber terminates at the end of the curved offset element on to a lens which throws the light into the oral cavity. The intra oral portion of the blade is a flat element which has a gentle curve on the longitudinal axis to enhance the area or the operating field. The length and width of the blade vary to suit the size of the oral cavity. The typical size currently designed is 50 × 10, 75 × 15, 100 × 20 mm (Length × Breadth). This corresponds to 00, 0, and 1 sized blade currently in use. The newly designed NOBL scope was subjected to scientific study for proving its worth.
Proof of concept study
We conducted a randomized control trial on manikin comparing the conventional Miller blade laryngoscope with our new NOBL scope.[6] 20 volunteers with various levels of experience in neonatal care participated in the study.
The objectives were, primarily to compare the pressure exerted on the upper lip of the mannequin between pediatric laryngoscope and NOBL scope and to compare the area of vision between pediatric laryngoscope and NOBL scope. Secondary objectives were to compare the area of pressure impression and time taken for intubation between pediatric laryngoscope and NOBL scope.
RESULTS 2
The frequency of pressure indentation on the maxilla was reduced by 45% with NOBL scope. The median (IQR) pressure exerted on the upper jaw with the conventional laryngoscope was 455 KPa (350–526) and that with NOBL scope was 80 KPa (0–134). The area of pressure indentation and time taken to intubate was significantly lower with the NOBL scope. We used photographic technique to measure the area of vision blocked while intubating. The area of vision blocked by conventional laryngoscope was 38.5% of the oral orifice compared to 12% with the NOBL scope [Figure 4]. About 95% of the participants agreed NOBL scope was easy to use.
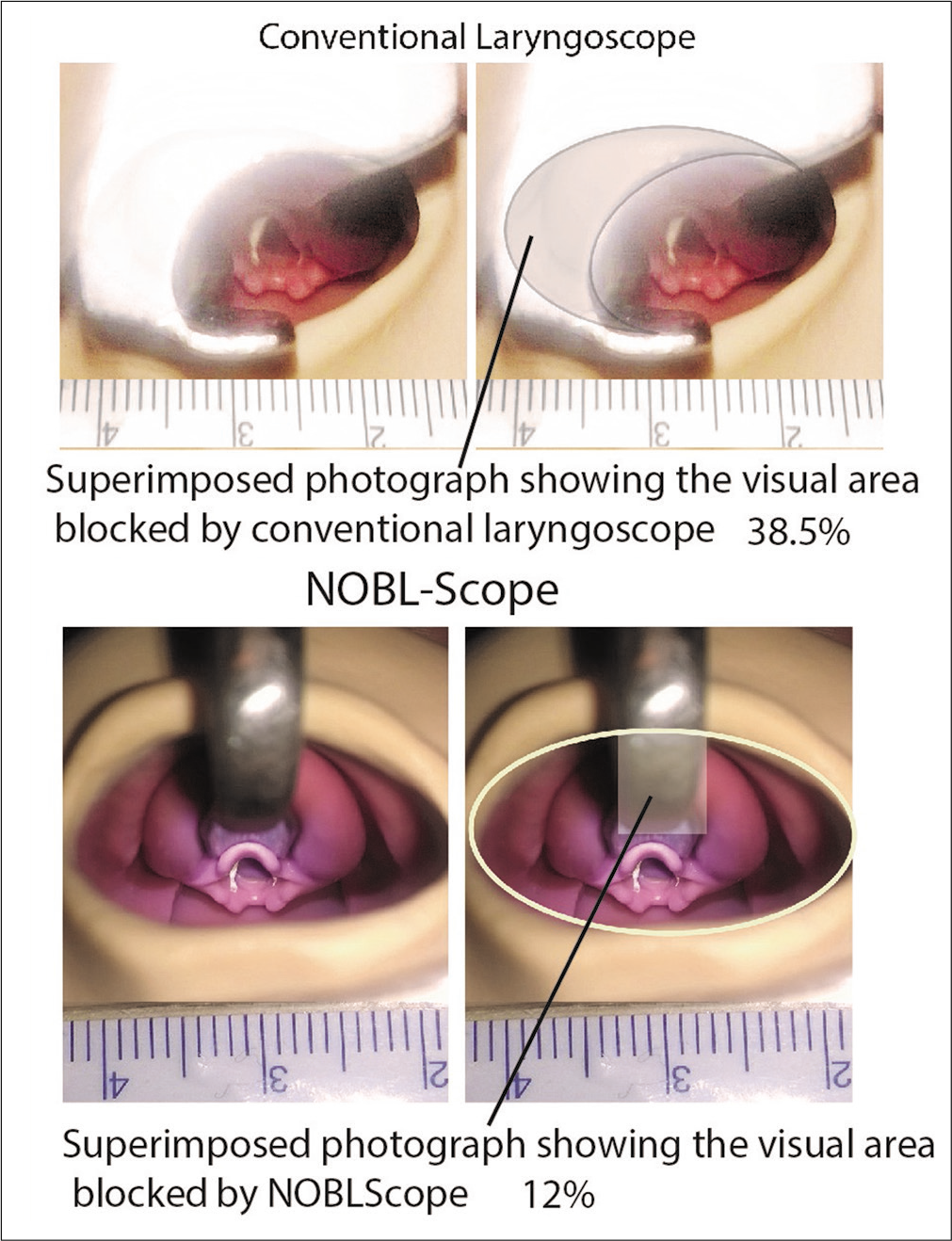
- Comparison of vision blocked by conventional pediatric laryngoscope and NOBL scope.
We had faced several challenges during the execution of the project. It was the diligent work of couple of engineers which made the design on the paper a reality as a product. Getting the unusual design manufactured was a huge challenge which was addressed using 3D print technology. Measuring the surface pressure on the manikin was another challenge. We used the pressure sensor films by Fujifilm to measure the pressures with appropriate experimental setup. The project was funded by Ontario Center of excellence, Canada.
DISCUSSION
Advances in the neonatal care have led to use of miniaturized adult laryngoscope in tiniest neonates. The pediatric and neonatologist community have endured the challenges these adopted laryngoscopes have thrown at us due to lack of purpose designed laryngoscope. Even the recent advances in video laryngoscopy have not improved the success rate of routine neonatal intubation.[7]
Conventional neonatal laryngoscope results in significant failure rate particularly among less experienced health-care providers.[1] It also results in trauma to the alveolar margin of the neonate leading to permanent damage to the dentition in future.[8-10] Our own study showed that the traumatic force exerted on the upper jaw during intubation was twice higher than the force determined to cause permanent histological damage in the animal models. The visual area is decreased by 38.5 to 48% depending on the oral cavity thus making the procedure difficult.
The new purpose designed NOBL scope do not have the hinge lock or the lateral flange seen in the traditional laryngoscope blade. The handle is attached to the blade at a distance away from the oral cavity and hence the visual area is significantly increased. The curved design of the horizontal offset element ensures the traumatic force exerted on the upper jaw is significantly reduced. Clinical study on cadaver is underway following which data on clinical safety will be available.
Intellectual property rights: It is especially important aspect of any innovation. The novelty has to be noted and certified by the appropriate agency so that the inventor can claim his/ her achievement for either economical or career benefit.
NOBL scope is patented under the author’s name in United States patent office. Patent No US 10,327,628, B2 date June 25, 2019.
Parting thoughts
Innovation is an inherent strength in every individual. It is the enlightenment of one’s own strength in problem solving. Many innovations which make our day-to-day life easier do so without much of fanfare. Hence, every scientific individual should embark on innovation for the progress of the science.
CONCLUSION
Neonatal intubation – can we make it better? Yes, we can!!
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Neonatal intubation: Success of pediatric trainees. J Pediatr. 2005;146:638-41.
- [CrossRef] [PubMed] [Google Scholar]
- The neonatal intubation causes defects in primary teeth of premature infants. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2013;158:605-12.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of tissue damage due to mechanical stresses. Int J Robot Res. 2007;26:1159-71.
- [CrossRef] [Google Scholar]
- Pediatric laryngoscopes and intubation aids old and new. Paediatr Anaesth. 2009;19:30-7.
- [CrossRef] [PubMed] [Google Scholar]
- Compression force on the upper jaw during neonatal intubation: Manikin study. J Paediatr Child Health. 2015;51:328-33.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of the Miller laryngoscope versus the prototype neonatal offset-blade laryngoscope in a manikin. Anaesthesia. 2016;71:320-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric video laryngoscope rescue for a difficult neonatal intubation. Paediatr Anaesth. 2008;18:790-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dental injuries resulting from tracheal intubation-a retrospective study. Dent Traumatol. 2009;25:73-7.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival and dental complications of orotracheal intubation. JAMA. 1976;236:957-8.
- [CrossRef] [PubMed] [Google Scholar]
- Defective primary dentition in survivors of neonatal mechanical ventilation. J Pediatr. 1980;96:106-8.
- [CrossRef] [Google Scholar]






