Translate this page into:
Acute leukoencephalopathy with restricted diffusion – Case Series
*Corresponding author: C. P. Ravi Kumar, Department of Paediatric Neurology, Aster CMI Hospital, Bengaluru, Karnataka, India. cpravikumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jyothi BN, Kumar CP, Kamble RB, Manivannan S. Acute leukoencephalopathy with restricted diffusion – Case Series. Karnataka Paediatr J. 2024;39:20-3. doi: 10.25259/KPJ_59_2023
Abstract
Acute leukoencephalopathy with restricted diffusion (ALERD) is a clinicopathological diagnosis that is characterized by severe encephalopathy and seizures with extensive areas of restricted diffusion in cerebral parenchyma. Case 1: Apparently healthy 13-month-old male child presented with acute febrile encephalopathy with a flurry of seizures with raised intracranial pressure. Investigations were consistent with multiorgan dysfunction along with severe metabolic acidosis, ketosis, and hyperammonemia. Initial magnetic resonance imaging (MRI) Brain was normal. However subsequent MRI brain suggested features of diffuse ALERD. With immunotherapy and supportive management, he improved and was discharged without sequelae. Case 2: A 9-month-old male child who was premorbidly normal presented with fever, status epilepticus, and encephalopathy. MRI Brain was suggestive of central sparing ALERD. He was discharged with sequelae with the advice of rehabilitation. Unfortunately, he got succumbed due to aspiration. Case 3: A 10-day-old neonate presented with the refusal of feeds, multiple seizures, and encephalopathy. MRI Brain revealed central sparing ALERD. Improved with immunotherapy and was developmentally normal at five months of age. ALERD is a clinic-radiological syndrome characterized by acute encephalopathy with restricted areas of diffusion in subcortical white matter on MRI. Reported two categories are Diffuse and Central sparing ALERD. Diffuse ALERD has severe manifestations. However, Case 1 had a good outcome, suggesting a variable prognosis. Central sparing ALERD is a milder form, but when basal ganglia are involved, it may have a worsened outcome, as seen in Case 2. Case 3 had central sparing ALERD, and had a good prognosis as described in literature. This study highlights the varied signs and symptoms of ALERD, including neonatal age of onset. Diagnosis is based on the restricted diffusion in white matter on diffusion-weighted imaging and the apparent diffusion coefficient in MRI of the brain. MRI may be normal in the initial course; hence, it’s important to repeat if strongly suspected. Prompt immunotherapy and supportive care are emphasised.
Keywords
Acute leukoencephalopathy with restricted diffusion
Apparent diffusion coefficient
Diffusion-weighted imaging
Immunotherapy
INTRODUCTION
Acute leukoencephalopathy with restricted diffusion (ALERD) is a clinical-radiological diagnosis that is characterised by severe encephalopathy and seizures with extensive areas of restricted diffusion in the bilateral cerebral parenchyma on magnetic resonance imaging (MRI).
ALERD is one of the infection-associated encephalopathy disorders reported in children.[1] According to the distribution of brain lesions, there are two varieties of ALERD: Diffuse ALERD with diffuse areas of restricted diffusion on MRI and central sparing ALERD, also known as Acute Encephalopathy with Biphasic Seizures and Late Reduced Diffusion.
Here, we report 3 cases with ALERD and review of literature on the same.
CASE SERIES
Case 1
A 13-month-old child who was previously healthy and developmentally normal child was admitted to another hospital with a history of fever for five days. He had status epilepticus on day 4 of illness, followed by encephalopathy. MRI Brain was normal on day 4 of illness. Despite being on two anti-seizure medications, he continued to have seizures. He had features of raised intracranial pressure. He was referred to our hospital for further management. At the time of presentation, he had an episode of hypoglycemia with high ammonia (650 m/dL), severe metabolic acidosis, substantially increased lactate, and encephalopathy. He had Multiorgan dysfunction involving the central nervous system (CNS), cardiac dysfunction, Acute liver failure with coagulopathy, and bone marrow suppression involving two cell lines. He was intubated due to shallow respiratory efforts, and hemodynamics were stabilised. Neuroprotective measures were taken, and titrated the Antiseizure medications accordingly. He was transfused with packed red blood cells and 2 pints of Fresh frozen plasma. He remained encephalopathic for the next 3–4 days and responded gradually. Repeat MRI brain on day 8 of illness showed a diffuse ALERD picture [Figure 1]. Blood culture, cerebrospinal fluid (CSF) analysis, culture, and meningoencephalitis panel were negative. EEG showed diffuse slowing with delta activity. Metabolic workup revealed a possibility of mitochondrial disease; however, it was dismissed after genetic workup. Gradually, he responded to the given treatment, and his sensorium improved. He was discharged on day 20 of illness with no neurological deficits.
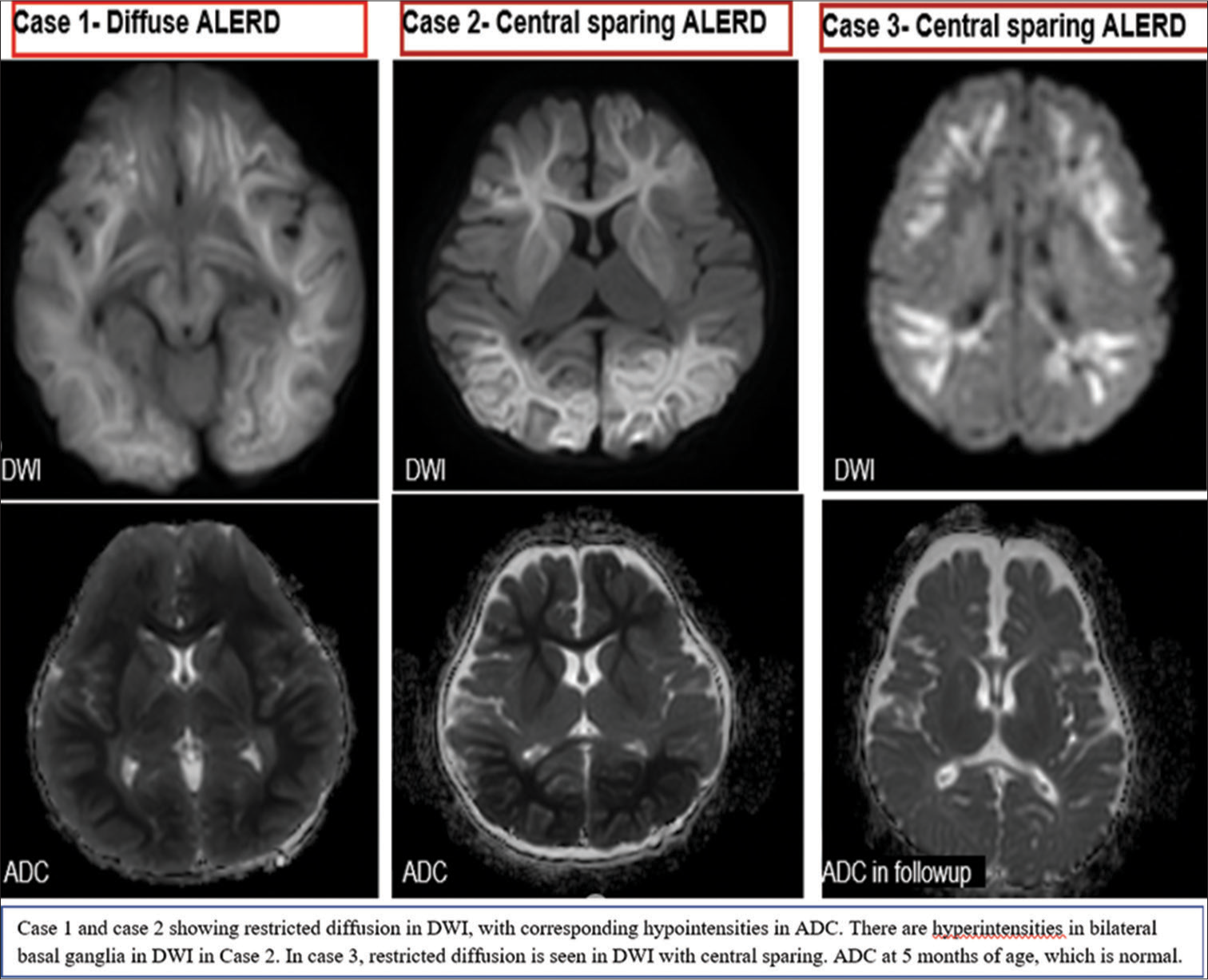
- ALERD: Acute leukoencephalopathy with restricted diffusion. DWI: Diffusion-weighted imaging, ADC: Apparent diffusion coefficient.
Case 2
A 9-month-old child was admitted to an elsewhere hospital with a history of fever on and off for 3–4 days multiple episodes of generalized tonic-clonic seizure with encephalopathy. He was treated with IV antibiotics, multiple Antiseizure medications, and neuroprotective measures. MRI Brain was normal on day 3 of illness. CSF analysis and meningoencephalitis panel were normal. In view of Persistent encephalopathy, he was referred to our hospital on day 8 of illness. On arrival, he was encephalopathic and had poor respiratory efforts. Hence, he was intubated and continued on ventilatory support. Relevant blood investigations were normal, except positivity for Dengue immunoglobulin M. Repeat MRI brain showed a picture of Central sparing ALERD [Figure 1]. He remained seizure-free for four days and again developed multiple episodes of focal seizures. Gradually, he was weaned off from ventilatory support after stabilization. He showed a very slow recovery with significant cortico-visual impairment and weak swallowing. Hence, he was discharged with an NG tube for feeds and with early intervention therapies. The very next day, he was presented with status epilepticus with cyanosis. Managed accordingly and discharged after three days. Unfortunately, after one week, he presented to the emergency room with sudden unresponsiveness, cessation of breathing, and cyanosis. Despite the best resuscitatory measures, he could not be revived!
Case 3
A 10-days-old neonate, born to a non-consanguineous couple, 2nd issue, with no significant antenatal and perinatal history, with a birth weight of 3 kg, was brought with complaints of refusal to feeds, which was followed by four episodes of right focal tonic-clonic seizures and encephalopathy. He was loaded with phenobarbitone and Levetiracetam. Basic blood investigations were within normal range. The Sepsis screen was negative. CSF analysis, culture, and Meningoencephalitis Panel, including enterovirus, were negative. He was treated empirically with antibiotics. MRI brain revealed central sparing ALERD. Blood Tandem mass spectrometry (TMS)was negative. He improved gradually and was discharged on day 17 of life with Levetiracetam. During follow-up, at five months of age, development was age-appropriate with no focal neurological deficits. The repeat MRI brain was normal [Figure 1].
DISCUSSION
ALERD is a clinicopathological syndrome characterized by acute encephalopathy with restricted areas of diffusion in subcortical white matter on MRI.[1] Infectious ALERD develops after infections, while toxic ALERD occurs on exposure to poisons, drug abuse, and cranial radiation, as described by Kamate.[1]
There are two different categories of brain lesions, namely Diffuse ALERD and Central sparing ALERD, based on their distribution.
Diffuse ALERD is a severe manifestation characterised by rapid deterioration of consciousness with shock and multiorgan dysfunction, leading to Coma. It’s associated with a guarded prognosis and can be associated with mortality. Neurosequelae are in the form of cognitive impairment, epilepsy, and behavioral problems. Case 1 had diffuse ALERD and presented with refractory status epilepticus, Coma, shock, Multiorgan dysfunction syndrome, had a malignant clinical course, and was discharged without neurological sequelae. This shows the variable prognosis of ALERD.
Central sparing ALERD is a relatively milder form. These patients have a biphasic clinical course. Onset is frequently characterised by fever status epilepticus followed by improved sensorium. Coma is rare, and a variable degree of cognitive impairment is noticed. Two of our cases had central sparing ALERD. 2nd case presented with shock, status epilepticus, and biphasic seizures. He was discharged with neurological sequelae in the form of dystonia and dysphagia. He succumbed after two weeks of discharge due to breakthrough seizures and cardiorespiratory arrest. A possibility of aspiration or sudden unexplained death in epilepsy was considered. Despite the central sparing type of ALERD, this child had neurological sequelae and died. This can be explained by the involvement of bilateral basal ganglia, which is a predictor of poor prognosis[2,3] also the delay in initiation of diagnosis-specific treatment (Steroids and IVIG started on day 8 of illness). This prompts the importance of early management in the case of ALERD.
Case 3 had a stormy course in NICU with biphasic seizures, discharged without sequelae. During follow-up at five months of age, his development was age-appropriate and with normal MRI findings. This showed a favourable prognosis as described in the literature—a first-ever reported case of ALERD in the neonatal age group, according to the best of our knowledge.
As described in the literature, central sparing ALERD is in the common form in our case reports.[2,3]
In a cohort of Japan study, which included 44 patients, the causative pathogens isolated were human herpesvirus-6, adenovirus, rotavirus, influenza virus, Mycoplasma pneumoniae, Enterovirus type Coxsackievirus A6, Escherichia coli O157:H7, and Streptococcus pneumonia.[4] In our case reports, no organism was isolated in two, and one had dengue infection. The absence of etiological organisms can be explained by the hypothesis put forward by Okumura et al.[5] that the pathophysiology doesn’t require direct CNS infection.
All 3 cases presented with prolonged multiple seizures and status epilepticus. One of the pathophysiological mechanisms for prolonged seizures and poor outcomes in people with ALERD has been identified as excitotoxic injury caused by excessive glutamine release.[6]
MRI is usually normal at the initial presentation, and once the disease progresses, it shows restricted diffusion in diffusion-weighted imaging (DWI) sequences. The changes in conventional sequences like T1 weighted, T2 weighted, and fluid-attenuated inversion recovery are very subtle to diagnose ALERD and are frequently missed. Signal alterations are more prominent on DWI sequences with substantially restricted diffusion (or hyperintensities) and edematous changes throughout the cortical and subcortical areas that show hypointensities in apparent diffusion coefficient (ADC) maps, which is diagnostic of ALERD.[1]
Case 1 and case 2 had normal initial MRI findings, where a repeat MRI was performed in view of persistent encephalopathy, which revealed a picture of ALERD. This would prompt the importance of repeat MRI if a high suspicion were made, as postulated by Kamate.[1]
In cases of ALERD, dextromethorphan, an antagonist of the N-methyl-D-aspartate receptor, and cyclosporine A, an apoptosis inhibitor, have been used.[7] However, a large cohort of studies are required.
All the 3 cases were treated with a pulse dose of methylprednisolone. Cases 1 and 2 required IV Immunoglobulins in view of poor progress.
CONCLUSION
This study highlights the varied signs and symptoms of ALERD, including neonatal age of onset.
Diagnosis is based on the finding of restricted diffusion in white matter and/or cortex on DWI and ADC in MRI of the brain. MRI may be normal in the initial 3–4 days, and hence, it is important to repeat MRI if ALERD is a strong suspect in a given case.
Prompt immunotherapy and supportive care are emphasised. Diffuse ALERD has a poor prognosis as compared to the central-sparing type of ALERD. However, it’s variable.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Acute leukoencephalopathy with restricted diffusion. Indian J Crit Care Med. 2018;22:519-23.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of outcomes for acute encephalopathy with reduced subcortical diffusion. Sci Rep. 2020;10:9134.
- [CrossRef] [PubMed] [Google Scholar]
- Involuntary movements and Coma as the prognostic marker for acute encephalopathy with biphasic seizures and late reduced diffusion. J Neurol Sci. 2016;370:39-43.
- [CrossRef] [PubMed] [Google Scholar]
- Seizure characteristics of epilepsy in childhood after acute encephalopathy with biphasic seizures and late reduced diffusion. Epilepsia. 2015;56:1286-93.
- [CrossRef] [PubMed] [Google Scholar]
- Differences of clinical manifestations according to the patterns of brain lesions in acute encephalopathy with reduced diffusion in the bilateral hemispheres. Am J Neuroradiol. 2009;30:825-30.
- [CrossRef] [PubMed] [Google Scholar]
- Excitotoxicity in acute encephalopathy with biphasic seizures and late reduced diffusion. AJNR Am J Neuroradiol. 2009;30:132-5.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of dextromethorphan and cyclosporine for acute encephalopathy. Pediatr Neurol. 2013;48:200-5.
- [CrossRef] [PubMed] [Google Scholar]






