Translate this page into:
The mandibular distraction osteogenesis; the key dental technique to success in a neonate with Pierre Robin’s sequence – A case report
*Corresponding author: H. A. Venkatesh, Department of Neonatology, Manipal Hospital, Bengaluru, Karnataka, India. venkatveena46@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Venkatesh HA, Shubha HV, Rao KS, Venkatesh S. The mandibular distraction osteogenesis; the key dental technique to success in a neonate with Pierre Robin’s sequence – A case report. Karnataka Paediatr J. 2024;39:34-6. doi: 10.25259/KPJ_61_2023
Abstract
A 15-day female neonate term small for gestational age with Pierre Robin Sequence was presented with respiratory distress, requiring respiratory care. The mandibular distraction surgery was performed for micrognathia and progressive respiratory distress. Gradually, she improved and was discharged home on gastrostomy tube feeding. This case underscores the importance of dentistry in the neonatal management of complicated Pierre Robin Sequence successfully.
Keywords
Neonate
Pierre robin sequence
Mandibular distraction osteogenesis
Dentistry
INTRODUCTION
Pierre Robin’s sequence is a congenital malformation seen in neonates causing respiratory morbidity. Many milder forms need a prone position and do well gradually. The severe forms may need a novel technique called mandibular distraction osteogenesis for the growth of the mandible, as it was used in our index case as a ray of hope.
CASE REPORT
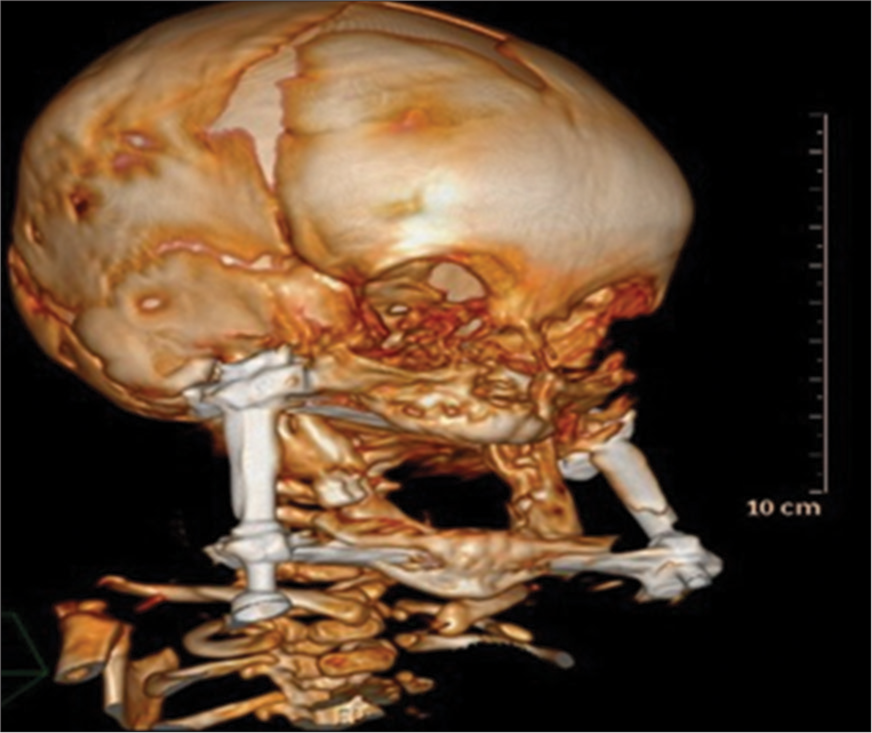
A term small for gestational age born to a non-consanguineous couple was presented with dysmorphic features such as a small chin, retrognathia and cleft palate [Figure 1]. She required resuscitation – delivery room continuous positive airway pressure (CPAP) and required ventilation for progressive respiratory failure. She was continued on the respiratory support and could not be weaned. Her upper airway was evaluated using bronchoscopy and demonstrated severe laryngomalacia needing aryepiglottoplasty. She continued to be on the respiratory support and in the prone position with no improvement in the respiratory condition. The maxillofacial surgeon opined the benefit of performing mandibular distraction osteogenesis (MDO) procedures. The computed tomography (CT) imaging of the mandible was performed before the procedure [Figure 2]. Post-procedure, the screw distraction of 1 mm/day for one week and then 2 mm up–39 mm over a period of 20 days. Gradually, she improved and could be weaned from the ventilator to CPAP and then to room air. The mandibular distractor was kept in situ for three months [Figure 3] until the repeat CT mandible showed adequate density of the bone [Figure 4].

- The neonate with micrognathia and retrognathia.

- Micrognathia with mandible distraction device fixed.

- The computed tomography scan of head and neck showing small and retro mandible before the device placement.
- Computed tomography scan of head and neck showing the lengthening of mandible after a period of device placement.
The feeding management included gastrostomy tube feeding in the initial phase and gradually started enteral feeds. The follow-up clinic demonstrated adequate growth and development. At around eight months of age, she underwent cleft palate closure.
DISCUSSION
The retro positioning of the tongue and hypoplasia of the mandible is an abnormality that causes airway obstruction in Robin’s syndrome and was first described in 1934.[1] The severe airway obstruction happens in around 23% of neonates, with Robin’s sequence requiring surgical intervention. In around 40–70% of cases, the airway obstruction is relieved by nursing the baby prone.[2-4] The nasopharyngeal airway relieves obstruction in some cases until the mandible grows.[5,6] Our index case had stridor secondary to severe laryngomalacia requiring CPAP and later needed aryepiglottoplasty. The prone nursing, nasopharyngeal airway, CPAP and aryepiglottoplasty did not relieve airway obstruction. The tracheostomy would be the historical treatment of such neonates. The mortality and morbidity, the difficulties in taking care, the long time required for decannulation and its impact on language and speech have limited this procedure and, hence, not been considered.
The MDO gained importance recently in the management of airway obstruction. Initially, this procedure was performed in patients failing tracheostomy and or tongue lip adhesion.[7,8] This technique lengthens the mandible, bringing the tongue forward and addressing both micrognathia and glossoptosis in relieving airway obstruction. This has become a promising therapy in most of the centres. The procedure requires a specialised person trained in the technique and is performed in phases. The device placement and osteotomy followed by the active distraction of 1–2 mm/day until 35–40 mm is achieved. Once the distraction was completed, the device was left for 4–6 weeks for the consolidation of regenerated bone.
In the index case, the MDO procedure was performed on day 90 after performing the CT head and neck to know the mandibular size, and later, gradually she was weaned from the ventilator to CPAP after two weeks of the procedure. Here the distraction device with the two screws was attached to the mandible after the incision and its separation. The screw was turned 1 mm every day for one week and 2 mm later for 20 days till around 40 mm, and then the device was kept for another four weeks without any distraction. The turning of the screw after the surgery will further separate the bone. The device was later left in situ for four weeks without screwing. The procedure, though safe, can be associated with complications, including damage to inferior alveolar nerves, infections, failure of distraction and the dislodgment of the device. In our case, none of the complications arose. There are different devices used in the mandibular distraction procedure – the external and the internal. The external device fixation was performed in our case. Post-MDO, her oxygenation improved. She was weaned gradually from CPAP to room air. The feeding gastrostomy was inserted as she did not tolerate the tube feeding and was discharged home on gastrostomy tube feeding for a couple of months. And was removed once the oral feed was established. The follow-up CT of the head and neck demonstrated the grown-up chin, and the device was removed. Currently, she is on full oral feeds with adequate weight and demonstrating normal milestones.
CONCLUSION
This case underscores the importance of dentistry in the neonatal management of complicated Pierre Robin Sequence successfully.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Glossoptosis due to atresia and hypotrophy of the mandible. Am J Dis Child. 1934;48:541-7.
- [CrossRef] [Google Scholar]
- Prognosis of airway obstruction and feeding difficulty in the Robin sequence. Int J Pediatr Otorhinolaryngol. 2005;70:319-24.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and severity of obstructive sleep apnea and snoring in infants with Pierre Robin sequence. Cleft Palate Craniofac J. 2011;48:614-8.
- [CrossRef] [PubMed] [Google Scholar]
- Airway management in patients with isolated Pierre Robin sequence during the first year of life. J Craniofac Surg. 2003;14:462-7.
- [CrossRef] [PubMed] [Google Scholar]
- The successful use of the nasopharyngeal airway in Pierre Robin sequence: An 11-year experience. Arch Dis Child. 2012;97:331-4.
- [CrossRef] [PubMed] [Google Scholar]
- Management of infants with Pierre Robin sequence. Cleft Palate Craniofac J. 2003;40:180-5.
- [CrossRef] [PubMed] [Google Scholar]
- Distraction osteogenesis in Pierre Robin sequence and related respiratory problems in children. J Craniofac Surg. 2002;13:79-83.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular distraction osteogenesis in very young patients to correct airway obstruction. Plast Reconstr Surg. 2001;108:302-11.
- [CrossRef] [PubMed] [Google Scholar]






