Translate this page into:
Malignant peripheral nerve sheath tumour in a child with neurofibromatosis type 1
*Corresponding author: Thirunavukkarasu Arun Babu, Department of Pediatrics, All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India. babuarun@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Balakrishnan P, Arun Babu T. Malignant peripheral nerve sheath tumour in a child with neurofibromatosis type 1. Karnataka Paediatr J. doi: 10.25259/KPJ_50_2024
Dear Editor,
Neurofibromatosis-1 (NF-1), an autosomal dominant inherited disorder caused by a mutation in the tumour suppressor gene NF1 on chromosome 17q.[1] Malignant peripheral nerve sheath tumour (MPNST) is a soft tissue sarcoma that arises from the peripheral nerve sheath or exhibits peripheral nerve sheath differentiation.[2] The incidence of MPNST in the general population is approximately 0.017 per 1 million persons per year, whereas in patients with NF-1, it is about 1 in 3,500. We report a rare case of MPNST with multiple systemic defects in a child with NF-1.
A 10-year-old male child, born out of a second-degree consanguineous marriage, presented with a swelling in the left supraclavicular region for 4 months. The swelling was painful, rapidly increasing in size, associated with tingling, numbness in the left upper limb and an inability to abduct the limb. Parents reported poor speech development and poor school performance. The father had multiple café-au-lait spots and neurofibromas on the trunk.
On general examination, the child was conscious but exhibited poor developmental skills for his age. Multiple café-au-lait spots were observed over the trunk and extremities, along with a plexiform neurofibroma on the left elbow [Figure 1a], drooping of the left shoulder, bilateral cryptorchidism, bilateral gynaecomastia, left eye exotropic squint and scoliosis of the lumbar vertebrae. A hard, tender, immobile swelling measuring 6 × 6 cm was noted in the left supraclavicular region [Figure 1b].
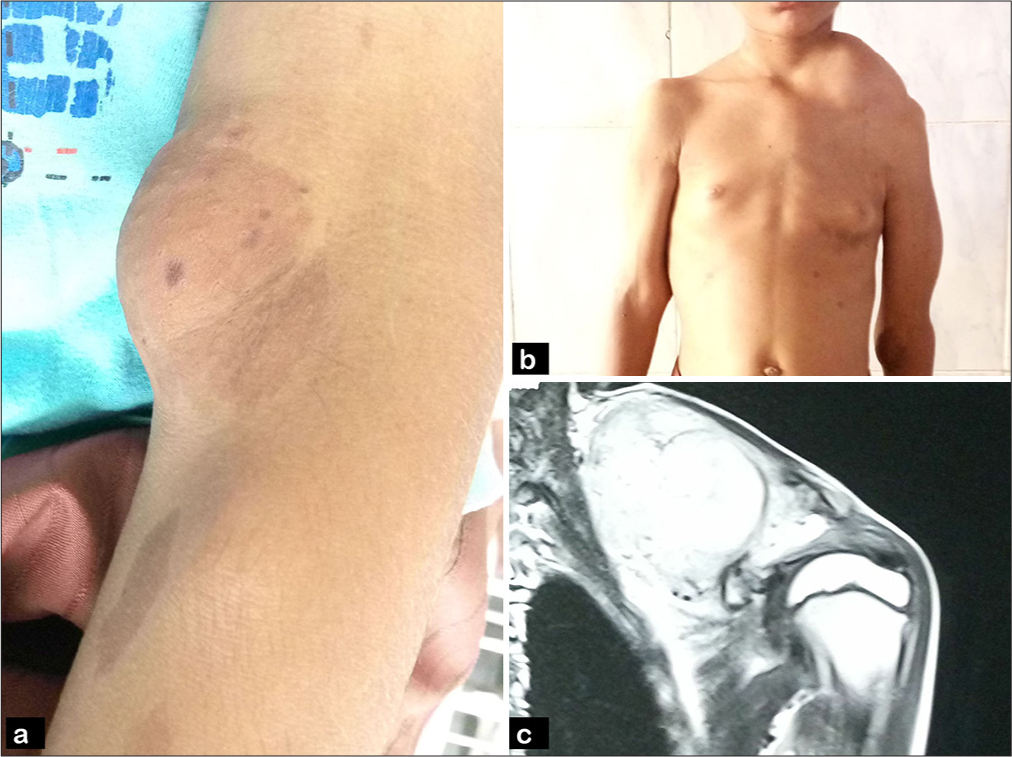
- (a) Picture shows plexiform neurofibroma in left arm and café-au-lait spots, (b) picture of trunk shows swelling in the left supraclavicular region, (c) magnetic resonance imaging shows soft tissue density lesion.
Magnetic resonance imaging revealed a lobulated soft tissue lesion with focal cystic areas measuring 6.5 × 6.5 × 4.5 cm in the intermuscular plane of the left supraclavicular and infraclavicular region, indenting the brachial plexus [Figure 1c]. Fine needle aspiration cytology showed atypical spindle cells with scant eosinophilic cytoplasm, pleomorphic hyperchromatic nuclei arranged in fascicles and sheets, nuclear palisading, atypical mitotic figures and a hemorrhagic myxoid background [Figure 2a]. Computed tomography of the abdomen and lungs showed no evidence of metastasis.
A biopsy of the lesion confirmed atypical spindle cells with scant cytoplasm, pleomorphic hyperchromatic nuclei arranged in fascicles and a herringbone pattern, atypical mitotic figures (4/10 High power fields) and necrosis [Figure 2b and c]. Immunohistochemistry revealed tumour cells negative for S100, transducer-like enhancer of split 1 (TLE-1), cytokeratin, desmin and human melanoma black 45 (HMB-45), but positive for nestin. Ultrasound of the abdomen showed bilateral testes within the inguinal canals.
![(a) Fine needle aspiration cytology (FNAC) shows atypical spindle cells with scant eosinophilic cytoplasm and pleomorphic hyperchromatic nuclei arranged in fascicles (hematoxylin and eosin [H&E stain, ×40]). (b) Histopathology showed atypical spindle cells with scant cytoplasm and pleomorphic hyperchromatic nucleus arranged in fascicles (H&E stain, ×40) and (c) previous image in ×400.](/content/113/2025/0/1/img/KPJ-50-2024-g002.png)
- (a) Fine needle aspiration cytology (FNAC) shows atypical spindle cells with scant eosinophilic cytoplasm and pleomorphic hyperchromatic nuclei arranged in fascicles (hematoxylin and eosin [H&E stain, ×40]). (b) Histopathology showed atypical spindle cells with scant cytoplasm and pleomorphic hyperchromatic nucleus arranged in fascicles (H&E stain, ×40) and (c) previous image in ×400.
A diagnosis of MPNST was made based on the clinical findings of neurofibromatosis and histopathological examination. The parents were counselled regarding the syndrome, surgical tumour resection, associated risks of haemorrhage and nerve palsy, radiotherapy and the potential for recurrence and metastasis. However, they did not consent to surgical excision. Later, the child was discharged at their request and was lost to follow-up.
The diagnosis of NF-1 in this child was based on the National Institute of Health criteria, with the patient meeting three of the seven criteria described.[3] Cognitive deficits and academic difficulties, common neurological issues in NF-1 patients, correlated with our case.[4]
Bilateral cryptorchidism and associated bilateral gynecomastia in NF-1 are uncommon and remain unexplained. MPNST occurring in the first decade of life is rare and, in this case, causes severe mass effects on the clavicle and brachial plexus in a short duration. Notably, the negativity of tumour cells for S100 and positivity for nestin, a novel and sensitive marker, helped confirm the diagnosis of MPNST.[5]
Patients with neurofibromatosis should be screened and followed up for MPNST to enable early diagnosis and management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Peripheral nerve tumors in neurofibromatosis 1: An overview on management and indications for surgical treatment in our experience. Neurol India. 2019;67:S38-44.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant peripheral nerve sheath tumour of transverse colon with peritoneal metastasis: A case report. J Med Case Rep. 2019;13:15.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant peripheral nerve sheath tumour (MPNST) of mandible: Solving the perplexity. BMJ Case Rep. 2015;2015:bcr2014207790.
- [CrossRef] [PubMed] [Google Scholar]
- Seizure, spinal schwannoma, peripheral neuropathy and pulmonary stenosis-A rare combination in a patient of Neurofibromatosis 1. Ann Indian Acad Neurol. 2012;15:51-3.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant peripheral nerve sheath tumours: Differentiation patterns and immunohistochemical features-a mini review and our new findings. J Cancer. 2012;3:303-9.
- [CrossRef] [PubMed] [Google Scholar]





