Translate this page into:
Admission trends, associated factors and the outcomes for children hospitalised to paediatric intensive care unit for asthma – A population based longitudinal study
*Corresponding author: Alok Kumar, Department of Pediatrics, University of West Indies, Bridgetown, Barbados. alok.kumar@cavehill.uwi.edu
-
Received: ,
Accepted: ,
How to cite this article: Krishnamurthy K, King R, Oredein B, Kumar A. Admission trends, associated factors and the outcomes for children hospitalised to paediatric intensive care unit for asthma – A population based longitudinal study. Karnataka Paediatr J. 2024;39:125-9. doi: 10.25259/KPJ_22_2024
Abstract
Objectives:
This study aims to quantify the burden of pediatric intensive care unit (PICU) admissions from acute severe asthma and to describe the associated factors and outcome in these admissions.
Material and Methods:
This was a prospective longitudinal population based study from 2015 through 2019. Included all children (< 16 years) with acute severe asthma who needed hospitalization. Ethical approval for the data collection was obtained. Real time hospital admission date was collected by one of the authors. The medical records of the patients were examined as per the objectives of the study.
Results:
From among the 13407 Emergency Room visits from acute asthma during study period, there were 1748 (13.0%) required hospital admissions and 101 (0.8%) including 66 (65.3%) males and 35 (34.7%) females were admitted to the PICU. Of the PICU admissions, 76 (75.2%) and 47 (46.5%) had previous hospitalization and PICU admissions respectively. Among those admitted to PICU 29 (28.7%), 61 (60.4%) and 11 (10.9%) were on daily inhaled corticosteroids (ISC), were non-compliant with their inhaled corticosteroids (ICS) and were not on any ICS. There was no mortality from asthma during the study period.
Conclusions:
The majority of the PICU admissions for acute asthma was among children with previous asthma hospitalization and those who did not use ICS or did not comply with ICS.
Keywords
Asthma
Paediatrics
Intensive care unit
INTRODUCTION
Asthma is one of the most prevalent non-communicable diseases in paediatric age group globally.[1] It carries a significant risk of morbidity and mortality, especially among children and adolescents.[2-4] Severe acute asthma is defined as an asthma exacerbation refractory to the usual therapy and accounts for up to 20% of all admissions to the paediatric intensive care unit (PICU) worldwide.[5,6] Over the past years, the frequency of PICU admissions for acute severe asthma has shown a significant rise in many countries.[5,6] Hospitalisation due to asthma is one of the most common ambulatory care-sensitive preventable admissions in children.[7-9] This may reflect the failure of appropriate, timely treatment, which is a predictor of the general management of asthma in the community.
Barbados, one of the countries in the Caribbean region of the Americas, has a population of 301,865 (2021 est.), with 17.5% of the inhabitants below 15 years of age (2021 est.). The infant mortality rate is 10.23/1,000 live births; life expectancy at birth, at 78.3 years, is amongst the highest of the Caribbean islands.[10] The literacy rate in this country is nearly 100%.[10] The health care indicators of Barbados are at par with the developed world. The country provides free health care for all residents.[11-13]
Barbados has one of the highest prevalences of asthma in the world, with a mean of 10,348 cases seen at the emergency clinic per year, as reported by Depradine and Lovell in 2015, and a 31.1% prevalence of recurrent wheezing amongst toddlers, as reported by Kumar et al. in 2021 for an estimated population of 284,000, including 53,000 children under the age of 16 years.[14-16] Asthma carries significant morbidity and risk of hospitalisation in this country.[14-19] Despite the substantial disease burden, there is no published data regarding sick asthmatic children requiring intensive care admissions from the region. A better understanding of the epidemiology and healthcare utilisation by sick asthmatic children may be useful in devising strategies to help reduce the frequency, severity, and mortality from acute severe asthma. The aim of the present study was to examine the trends in PICU admissions from acute severe asthma in Barbados and to describe the associated factors and outcome of PICU admissions from acute severe asthma.
MATERIAL AND METHODS
Case definition
Paediatric asthma is characterised by persistent or recurrent respiratory symptoms such as wheezing, coughing, shortness of breath, and chest tightness. Severe acute asthma is an acute onset of severe and potentially life-threatening asthma symptoms that does not respond to usual treatment with bronchodilators and systemic corticosteroids.
Study design and period
The retrospective study was conducted on the data available from the PICU admission database from a single centre for the period from January 2015 to December 2019.
Study population and inclusion criterion
The PICU at the Queen Elizabeth Hospital (QEH) is the only such facility in Barbados that caters to the entire paediatric population of this country. Asthmatic children from 3 to 16 years of age who were admitted into the PICU at the QEH with any one of the following criteria was included in the study: persistent hypoxia (SPO2 <90% in room air and PaO2 <60 mmHg) or hypercarbia (Pa CO2 >50 mmHg), need for very frequent (<2 h) or continuous nebulisation therapy, signs of exhaustion with shallow respiration, altered mental state, air leak syndrome, or respiratory failure. Those children with acute severe asthma who died on arrival or died within 2 h of admission were not included in this study.
Study outcome
Independent variables such as age, gender, final diagnosis at discharge, comorbidities, history of past admissions to hospital and PICU for acute asthma, management details, length of intensive care unit stay, and the admission outcome were recorded.
Operational definition
Admission outcome indicates either the patient discharged or died at the time of discharge.
Length of PICU stay was defined as a period in days from admission time to discharge time.
PICU management included medications used for the control and reversal of the acute severe asthma, type and need for respiratory support needed if any and any complications.
PICU Mortality was calculated as the number of deaths from acute severe asthma divided by the total number of patients admitted with acute severe asthma.
Data collection protocols and procedures
The ethics approval was obtained before starting data collection from the Institutional Review Board at the Queen Elizabeth Hospital on 17 January 2015 (Ref: board201501). Patients were identified from the PICU admission registry. Data was extracted from the case records by investigators using a pre-designed data collection sheet. To ensure content validity, the questionnaire was adapted from previous related studies and suitably modified. The medical records of the patients were examined as per the objectives of the study.
Data collection and analysis
Data were collected manually, de-identified (anonymised), coded and entered into Epi info version 7 computer program. It was then exported to Statistical Package for the Social Sciences version 26.0 for analysis. Bivariable analysis was carried out to examine the effect of explanatory variables over the outcome variable. A P < 0.05 on bivariable analysis was considered significant. Strength of association was measured by an adjusted odds ratio with a 95% confidence interval (CI). Frequency, percentage, tables and figures were used to present the data.
RESULTS
There were a total of 12708 children who presented to the emergency room (ER) at the QEH during the 5 years study period. Of those presenting to the ER, 1748 children (13.8%; 95% CI = 13.2%, 14.4%) were admitted to the paediatric wards and 101 (0.7%; 95% CI = 0.6%, 0.9%) required PICU admission due to acute asthma. During the same period there were a total of 539 admissions to the PICU. The PICU admissions for acute severe asthma accounted for 18.7% (95% CI = 15.6%, 22.3%) of the total PICU admissions. Of those requiring PICU admissions, 24 (23.8%; 95% CI = 16.1%, 33.5%) were admitted directly from the ER while the remaining 77 (76.2%; 95% CI = 66.5%, 83.9%) were transferred from the ward after worsening of their clinical condition.
Trends in the proportion of children visiting the ER for acute asthma who required PICU admission are shown in Figure 1. Analysis of the trends in the PICU admissions rate (children with acute severe asthma requiring admission to PICU/total number of children with acute asthma presenting to the emergency care service) over the 5 year study period by Chi-square test returned a value of 0.1353 (non-direction) which was not significant. Trends in the proportion of the total PICU admissions that were from acute severe asthma (PICU admissions from acute severe asthma/total number of PICU admissions) as shown in Figure 2 were also not significant (P = 0.9513).
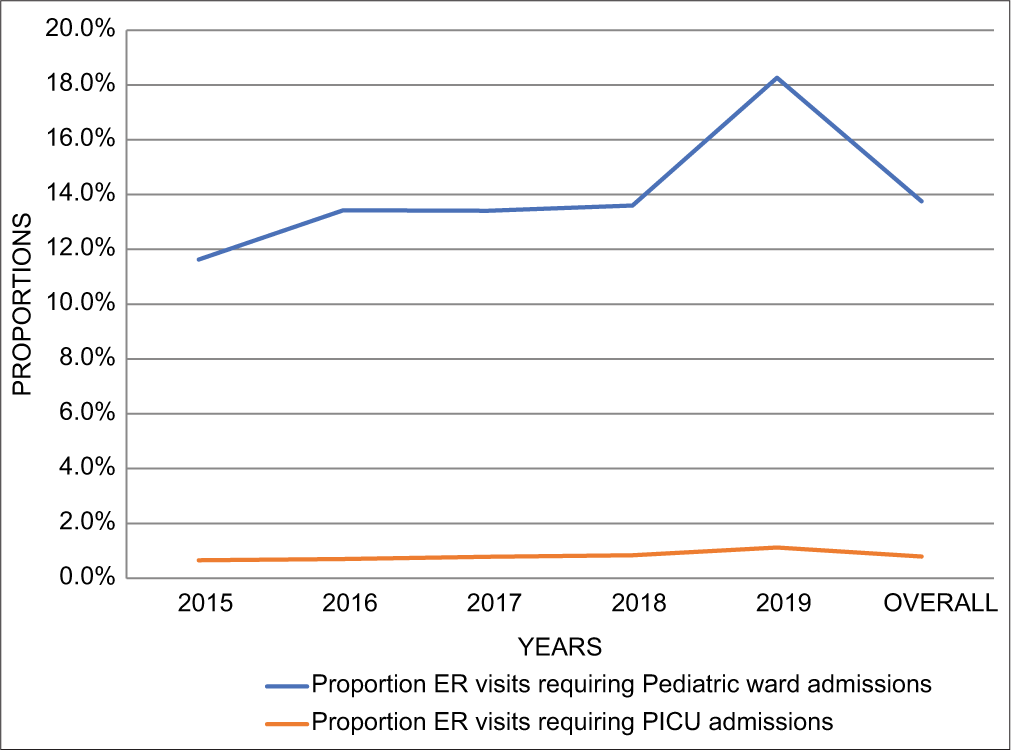
- Trends in the proportion of childhood asthma emergency room (ER) visits admitted to the paediatric general ward and the paediatric intensive care unit during 2015 through 2019 in Barbados. PICU: Paediatric intensive care unit.
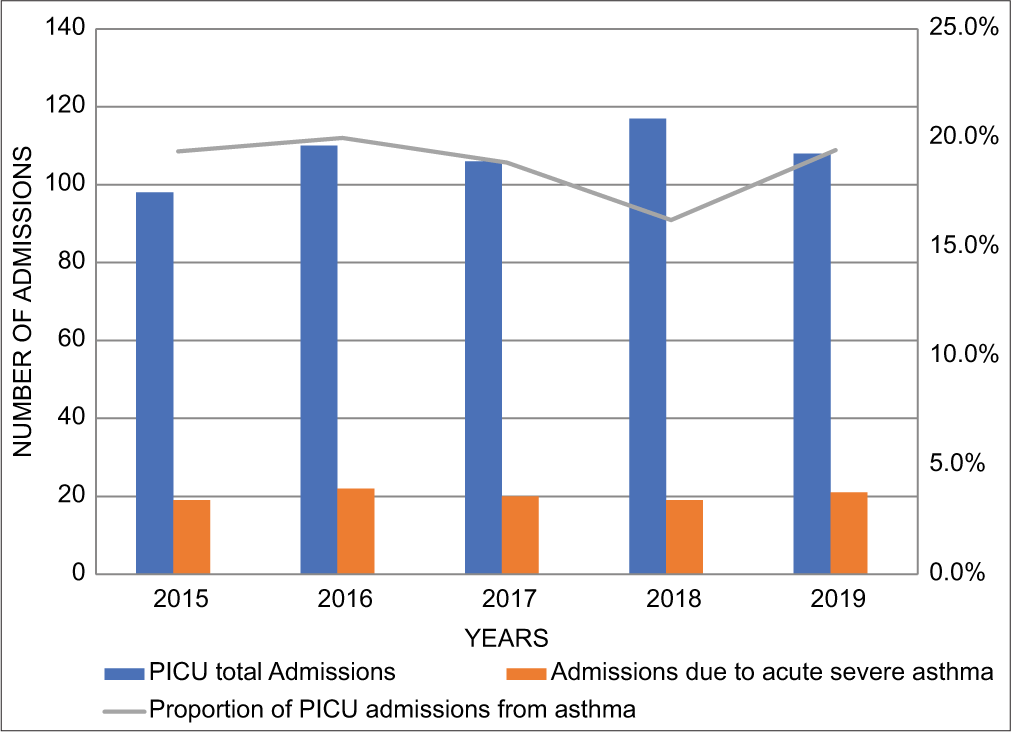
- Trends in the proportion of paediatric intensive care unit admissions from acute severe asthma during 2015–2029 in Barbados. PICU: Paediatric intensive care unit.
The demographic characteristics of the study population are shown in Figure 3. Of the 101 children admitted to the PICU for acute severe asthma, 49 (48.5%; 95% CI = 38.5%, 58.6%) were children younger than 5 years and 66 (65.3%; 95% CI = 55.2%, 74.4%) were males. Amongst the 49 under-5 children admitted to the PICU for acute severe asthma, 26 (53.1%; 95% CI = 38.4%, 67.2%) children had an additional diagnosis of pneumonia. Whereas of the 24 children in the age group 10 to <15 years who were admitted to the PICU with acute severe asthma, 6 (25%; 95% CI = 10.6%, 47.1%) had an additional diagnosis of pneumonia.
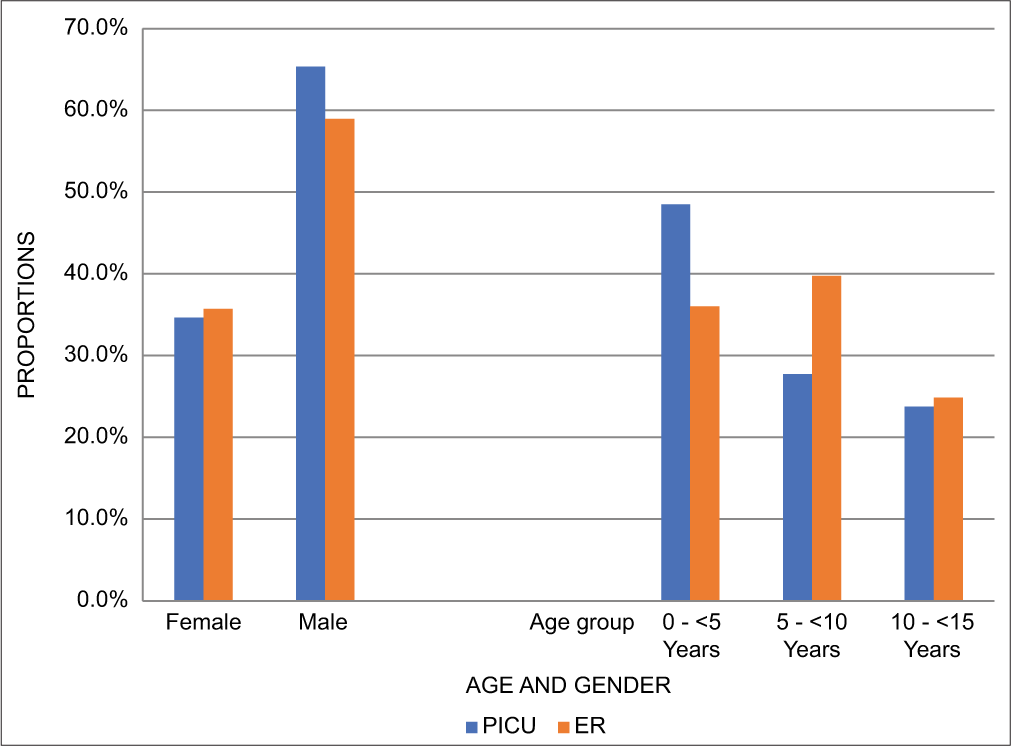
- Demography of children admitted to the paediatric intensive care unit and those presenting to the emergency room (ER) in Barbados. PICU: Paediatric intensive care unit.
Past asthma history of children admitted to the PICU for acute severe asthma is shown in Table 1. Overall 22 (21.8%; 95% CI = 14.4%, 31.3%) children were previously not known to have asthma but were prescribed bronchodilator medication in the past, and 18 (17.8%; 95% CI = 11.2%, 27.0%) were previously not known to have asthma and never prescribed bronchodilator medication in the past. Past treatment characterisation of 101 children admitted to the PICU for acute severe asthma is shown in Table 2. Overall 51 (50.5%; 95% CI = 40.4%, 60.5%) were non-compliant with their inhaled corticosteroid medication, and 21 (20.8%; 95% CI = 13.6%, 30.2%) were not prescribed any inhaled corticosteroids medication.
| Past asthma history | n=101 | % (95% confidence interval) |
|---|---|---|
| Previously known to have Asthma | 61 | 60.4 (50.1, 69.8) |
| Previously not known to have Asthma but was prescribed bronchodilator and corticosteroid medication in the past | 22 | 21.8 (14.4, 31.3) |
| Previously not known to have Asthma and never prescribed bronchodilator medication in the past | 18 | 17.8 (11.2, 27.0) |
PICU: Paediatric intensive care unit
| Previous asthma admission to general paediatric ward | 76 | 75.24 (65.5, 83.1) |
| Previous PICU admissions | 47 | 46.5 (36.6, 56.7) |
| On daily inhaled steroid and compliant | 29 | 28.7 (20.7, 38.7) |
| Non-compliance with inhaled steroid | 51 | 50.5 (40.4, 60.5) |
| Not on inhaled steroid | 21 | 20.8 (13.6, 30.2) |
PICU: Paediatric intensive care unit
Over all eight patients required intubation and ventilator support and there was one death in a 4-year-old child with asthma and bilateral bronchopneumonia and sepsis. Remaining 100 children admitted to the PICU for acute severe asthma during the study period were discharged from the PICU.
DISCUSSION
In this population-based study, we found that <1% of all children presenting to the ER for acute asthma required PICU admissions and a little over 5% of all hospital admissions for acute severe asthma were to the PICU. The reported proportion of the children admitted to the hospital for severe acute asthma that required PICU admission ranged from 5% to 25%.[5,6,20] However, a more recent 2023 study from the USA reported that 1.6% of children presenting with acute asthma required PICU admission and 5.6% of all asthma admissions in children were to the PICU.[21] These figures are similar to those of our findings in this study. Asthma being a common condition in this population, its management in the health care setting of this country is standardised and the standard of care is rigorously adhered to. Adequate standard care of children in our settings may be the reason for a lower rate of PICU admissions of children with severe acute asthma (SAA). We did not notice any trend in the PICU admissions for SAA in children in this study over the 5-year period. Increasing trends of PICU admissions for asthma as reported in some studies.[6,20,22]
The majority of the children who required PICU admissions for the SAA were in the age group 0–<5 years and nearly two-thirds were males. Similar observations have been made in other studies.[6,21,22] Of note nearly two third of these children had an additional diagnosis of bronchopneumonia. The role of viral respiratory infections in the exacerbation and severity of acute asthma has been well documented.[23,24] Lung infection in children could be a trigger for acute attack of asthma and may also exaggerate the impact of the acute asthma by further compromising oxygenation and overall well-being of these children. Furthermore, infectious conditions are more common in male children compared to females.
Another notable finding from this study was that over a fifth of the children admitted to the PICU for SAA were not known to be asthmatic to their parents, although they have had medications typically used to treat asthma. Diagnosis of asthma in young children is problematic and there are distinctly different asthma phenotypes in children. Due to the complexities surrounding asthma diagnosis in young children, physicians often do not provide asthma diagnosis to younger children. However, this may have compromised the adequacy of asthma management in these children and predisposed them for SAA. This may have reflected in the finding of over half of all the children admitted to the PICU for SAA in this study were non-compliant with their inhaled corticosteroids (ICS) inhalers and history of previous hospitalisation for SAA in the past in nearly half the cases. Similar findings have been reported in other studies.[6,25] However, recent studies have failed to support the lack of inhaled corticosteroids in the treatment or non-adherence to ICS as a risk factor for PICU admissions for SAA in children.[25,26]
CONCLUSION
A very small proportion of children with acute asthma who present to the emergency care facility are found to have severe acute exacerbation and require paediatric intensive care support. The majority of these children are under-5 males, have had inadequate asthma treatment in the past and have been hospitalised for asthma previously. The salient findings from this seminal study of PICU admission for SAA in children make a strong case for more comprehensive study of the risk factors for the SAA in children that necessitate PICU admission and how this could be prevented.
Ethical approval
The ethics approval was obtained from the Institutional Review Board at the Queen Elizabeth Hospital (Ref: board201501), on 17th January 2015.
Declaration of patient consent
Patient consent was not required as it is a retrospective clinical audit of PICU patients by the PICU consultant who provided the care.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Worldwide trends in the burden of asthma symptoms in school-aged children: Global Asthma network phase I cross-sectional study. Lancet. 2021;398:1569-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric asthma: A global epidemic. Ann Glob Health. 2019;85:6.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality and morbidity in children with asthma: A nationwide study in Korea. Respir Med. 2021;177:106306.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in asthma hospital admissions and mortality in Kuwait, 2000-2014: A national retrospective observational study. BMJ Open. 2018;8:e021244.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma changes at a pediatric intensive care unit after 10 years: Observational study. Ann Thorac Med. 2015;10:243-8.
- [CrossRef] [PubMed] [Google Scholar]
- Children with severe acute asthma admitted to Dutch PICUs: A changing landscape. Pediatr Pulmonol. 2018;53:857-65.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric quality indicators overview. Available from: http://www.qualityindicators.ahrq.gov/Modules/pdi_overview.aspx [Last accessed 2024 Feb 20]
- [Google Scholar]
- Measures of pediatric health care quality based on hospital administrative data. The pediatric quality indicators [Technical Report]. :1-137.
- [Google Scholar]
- Conditions for which onset or hospital admission is potentially preventable by timely and effective ambulatory care. J Health Serv Res Policy. 2000;5:222-30.
- [CrossRef] [PubMed] [Google Scholar]
- Barbados demographic profile. 2020. Available from: https://www.indexmundi.com/barbados/#google_vignette [Last accessed 2016 May 16]
- [Google Scholar]
- Brief presentation on the primary health care in Barbados. 2011. Available from: https://www3.paho.org/ecc/dmdocuments/Renewal%20of%20PHC%20in%20Barbados.pdf [Last accessed 2024 May 16]
- [Google Scholar]
- A review of the public-funded primary health care facilities for children in the pluralistic health care settings of Barbados, a Caribbean island. Prim Health Care Res Dev. 2016;17:157-65.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the role of the public and private funded primary health care facilities for children in a pluralistic health care setting of Barbados: One of the English Caribbean countries. Int J Prev Med. 2015;6:106.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of recurrent wheezing in infants and toddlers in Barbados: Findings from a prospective study of a cohort of babies born during 2015-2017. Allergol Immunopathol (Madr). 2021;49:17-24.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between African dust carried in the Atlantic trade winds and surges in pediatric asthma attendances in the Caribbean. Int J Biometeorol. 2008;52:823-32.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of hospitalizations and mortality from acute severe asthma among children in Barbados, 2013-2016 In: 64th Annual CARPHA Health Research Conference, Port of Spain. 2019.
- [Google Scholar]
- Avoidable hospitalization of children from ambulatory care sensitive conditions in Barbados: A measure of the access and uptake of primary health care. Health Prim Care. 2020;4:1-7.
- [CrossRef] [Google Scholar]
- Assessing a public health intervention for children in Barbados, 2003-2008. Prev Chronic Dis. 2015;12:E137.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in admissions for paediatric status asthmaticus in New Jersey over a 15-year period. Paediatrics. 2010;126:e904-11.
- [CrossRef] [PubMed] [Google Scholar]
- Initial emergency department vital signs may predict PICU admission in pediatric patients presenting with asthma exacerbation. J Asthma. 2023;60:960-8.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma in paediatric intensive care in England residents: Observational study. Sci Rep. 2022;12:1315.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric asthma and viral infection. Arch Bronconeumol. 2016;52:269-73.
- [CrossRef] [PubMed] [Google Scholar]
- Beyond respiratory syncytial virus and rhinovirus in the pathogenesis and exacerbation of asthma: The role of metapneumovirus, bocavirus and influenza virus. Immunol Allergy Clin North Am. 2019;39:391-401.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for intensive care admission in children with severe acute asthma in the Netherlands: A prospective multicentre study. ERJ Open Res. 2020;6:2-9.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for pediatric intensive care admission in children with acute asthma. Respir Care. 2012;57:1391-7.
- [CrossRef] [PubMed] [Google Scholar]






