Translate this page into:
Childhood lupus emergency presentation: Is early treatment justified: A case series
*Corresponding author: Abhijit Venkatesh Joshi, Department of Paediatrics, Chiranjeev Children’s Hospital and Critical Care Center, Aurangabad, Maharashtra, India. joshiabhijit71@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Khadke RR, Joshi AV, Kulkarni GL, Kulkarni MG. Childhood lupus emergency presentation: Is early treatment justified: A case series. Karnataka Paediatr J. 2024;39:24-7. doi: 10.25259/KPJ_48_2023
Abstract
Juvenile systemic lupus erythematosus is a multisystem disorder of autoimmune aetiology and is diagnosed on the basis of criteria such as the constitutional symptoms, various symptoms, and signs related to multi-system involvement and supporting laboratory investigations. It is sometimes very challenging when we come across some JSLE cases with an atypical presentation or as a catastrophe. We have discussed a few atypical cases of systemic lupus erythematosus here. Definitive diagnostic tests such as the anti-nuclear antibody with a high negative predictive value and other diagnostic tests would take time and it is worth starting treatment rather than waiting for the investigations in some cases. This case report study is to sensitise the treating paediatrician to use clinical acumen to plan meticulously the management of JSLE cases.
Keywords
Haemolytic anaemia
Autoimmune
Lupus vasculitis
Central nervous system
Retinal artery occlusion
INTRODUCTION
The diagnosis of systemic lupus erythematosus (SLE) becomes challenging due to the lack of definite pathognomonic features or tests. We have compiled clinical data of four interesting cases of childhood SLE which posed a diagnostic challenge. These cases had variable clinical presentations and a stormy course. The clinical data compiled includes the clinical presentation and diagnostic workup of these cases. This includes one case of unilateral central retinal artery occlusion, a case of autoimmune thrombocytopenia with haemolytic anaemia (Evan’s syndrome), a case of autoimmune haemolytic anaemia (AIHA), and a case of neuropsychiatric systemic lupus erythematosus (NPSLE). These cases posed problems for the diagnosis due to their stormy course and atypical presentation. A rapid treatment plan changed the outcome and prevented the deterioration of all patients. A delay in the diagnosis and urgent treatment would seriously jeopardize the outcome of all these cases.
We applied the European League Against Rheumatism/American College of Rheumatology 2019 criteria for SLE diagnosis with a positive anti-nuclear antibody (ANA) as the entry criterion and other criteria for fulfilling the diagnosis [Figure 1].[1]

- Adapted from 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. SLE: Systemic lupus erythematosus, C3: Complement 3, C4: Complement 4, *: Anti-double-stranded DNA (deoxyribonucleic acid) antibodies.
CASE SERIES
Case 1
A 16-year-old girl had symptoms in the form of polymenorrhagia and extreme weakness and a history of hair loss over 4 months. She presented with severe anaemia in cardiac failure and compatible blood of the same ABO and Rh type could not be arranged due to mismatch. She presented with nonscarring patchy alopecia, malar rash, and a rash over the neck with photosensitivity. Investigations revealed severe anaemia of macrocytic red cells, elevated indirect bilirubin level, a strong positive direct Coombs test, positive indirect Coombs test, and an elevated reticulocyte count pointing to AIHA. With a high index of suspicion for SLE, pending ANA report, she was treated with methylprednisolone in high doses followed by a maintenance dose of oral steroids and hydroxychloroquine. She recovered from severe anaemia without a blood transfusion. She showed a positive ANA by immunofluorescence. A positive double-stranded DNA antibody (anti-dsDNA) was also added to the diagnosis.
Case 2
A 12-year-old female presented to the emergency room needing mechanical ventilator support for breathlessness and parenteral fluids and inotropes for circulatory shock. She had a history of prolonged and heavy menstrual bleeding and severe weakness over 1 and ½ months. She presented with a characteristic malar rash over the face and a macular rash over the limbs. She had severe anaemia, leukopenia, and severe thrombocytopenia, with elevated reticulocyte count and a strong positive direct Coombs test. Her chest radiograph showed bilateral pulmonary infiltrates. Along with supportive care, she needed packed red blood cells, platelets transfusion, and steroids given initially in high doses. With a high index for suspicion of SLE with vasculitis, a further workup showed a positive ANA by IF, positive anti-dsDNA, low serum complement levels, and positive anti-SM antibody. She also had significant proteinuria and her planned kidney biopsy revealed class 3 nephritis. Cyclophosphamide was started for the induction remission and she was put on low-dose steroids and hydroxychloroquine with advice to have a regular follow-up.
Case 3
A 10-year-old boy was referred with pain in the digits and feet with peeling of skin over palms over 1 month followed by sudden dimness of vision in the left eye. He also had a fever over 4–5 days which was not attributed to any infective aetiology. His general examination showed hypertension. His left eye fundus showed macular oedema, haemorrhages around the disc, tortuous blood vessels, and cherry red spots [Figure 2]. On investigations, he had anaemia, raised C-reactive protein, and significant proteinuria. His coagulation profile including prothrombin time, activated partial thromboplastin time protein-C activity, protein-S activity, and antithrombin 3 was normal. By keeping the possibility of inflammatory multisystem disease with probable vasculitis, ANA by IF was done and turned positive, with a positive dsDNA antibody, low complement C3 and C4, and a high urinary protein to creatinine ratio. He was put on steroids, antihypertensive drugs, and acetylsalicylate. His kidney biopsy was planned later which showed class 2 nephritis. Cyclophosphamide was started as induction remission. There was a slight improvement in vision in the form of perception of light but his vision could not recover despite the continuation of treatment.
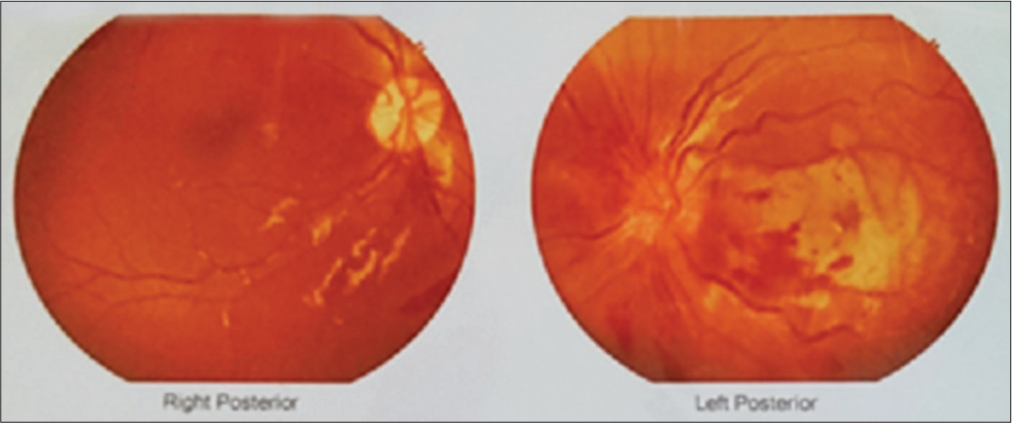
- Fundus Right eye: Normal, Left eye: tortuous blood vessels, hemorrhages around the disc, macular edema, cherry red spots, optic neuritis with retinitis with sub-foveal serous fluid.
Case 4
A 7-year-old girl presented to another hospital for a high intermittent fever for 2 months and was hospitalised for convulsions. She had generalised lymphadenopathy, and oral ulcers on clinical examination. Her investigations showed bicytopenia in the form of anaemia and thrombocytopenia. Cerebrospinal fluid had leukocytosis and computed tomography (CT) brain was reported normal. She was treated for tuberculous meningitis though specific tests for bacteriological confirmation were negative. She recovered partially from the illness but landed with us in status epilepticus with a fever. She needed mechanical ventilator support for respiratory failure and encephalopathy. She had hypertension and developed a macular rash over the body and had hepato-splenomegaly. The bicytopenia persisted and the repeat CT scan brain was normal. In v/o persistent fever, pancytopenia, and clinical picture s/o a non-infective aetiology, the possibility of lupus is kept in mind after a normal bone marrow examination. She was treated empirically for neurogenic lupus with steroids, and cyclophosphamide, pending the reports. Her ANA and anti-SM antibodies turned positive. She recovered and was seizure free and with an intact neurological status.
DISCUSSION
This case study report again highlighted that though AIHA as the initial presentation of underlying SLE is extremely rare,[2] a high index of suspicion for SLE as the cause is worthy [Table 1].[3] In both our cases of AIHA, the first was referred to us in cardiac failure with severe anaemia, and cross matching with compatible blood was not possible in view of positive direct agglutination test. This led us to search for the cause and yielded positive ANA and anti-DNA antibodies. The second case was with prolonged bleeding with thrombocytopenia and presented with pulmonary haemorrhage. This guided us to think of vasculitis as the cause. The lupus anticoagulant was negative and negative anti-CL antibodies ruled out antiphospholipid antibody syndrome. This was treated as SLE with severe thrombocytopenia causing pulmonary haemorrhage. A thorough work-up in AIHA will aid in the detection of underlying secondary conditions. The response rate to steroids in AIHA is reported to be around 80%.[4]
| ACR criteria | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| ANA | 1:1000 | 1:3200 | 1:320 | 2.23 index |
| Constitutional symptoms | Present | Present | Present | Present |
| Muco-cutaneous | Hair loss | Malar rash/photosensitivity | Absent | Rash/oral ulcers |
| Musculo-skeletal | Absent | Absent | Arthralgia | Absent |
| Neuropsychiatric | Absent | Absent | Headache Multiple hemorrhagic infarcts brain | Status epilepticus |
| Hematological | Immune hemolytic anemia | Immune hemolytic anemia/thrombocytopenia | Immune hemolytic anemia | Leukopenia/thrombocytopenia |
| Serositis (pleural/pericardial) | Absent | Pleural effusion/ascites | Pleuro-pulmonic pathology | Absent |
| Immunological | Low serum C3 and C4 | Low serum C3 and C4, positive ds-DNA and Sm antigen | Low serum C3 and C4, positive anti-ds-DNA | Absent |
| Renal | Absent | Class 2 nephritis | Class 2 nephritis | Hypertension Proteinuria |
ACR: American college of Rheumatology, ANA: Anti-nuclear antibody, C3 and C4-complement 3 and 4, ds-DNA: Double stranded DNA, Sm: Smith, EULAR: European league against rheumatism, SLE: Systemic lupus erythematosus.
Unilateral branch retinal artery occlusion (BRAO), though as the sole presentation of retinopathy is extremely rare in SLE, the only ophthalmological evaluation will not reveal the cause and other evidence for SLE has to be looked for. The child in our case had other features of SLE in addition to BRAO, such as macular rash, hypertension with proteinuria, and joint symptoms. This confirmed the diagnosis of SLE; the treatment was directed to SLE as a whole in the form of immunotherapy and only optical manoeuvres could not resolve the symptoms even if the main symptoms were in the retina.[5]
Only 25% of Juvenile-onset systemic lupus erythematosus patients present as NPSLE. The incidence of seizures at the initial presentation is only 25%.[4,5] With clinical features of NPSLE very variable and non-specific in children, the diagnosis is at times challenging and poses under-recognition and subsequent high rates of complications.[6,7]
CONCLUSION
These clinical scenarios show a series of difficult, at risk SLE cases with variable presentation posing a difficulty for the clinician to diagnose and manage with limited resources. A high clinical acumen and a high index of suspicion for SLE in these cases underlie the success with the help of an urgent treatment plan pending the investigation results. This study emphasises the need to put lupus high as the differential in such as haematological, neurological, and ophthalmological emergencies presenting to the emergency room.
The idea behind this article is to sensitise the clinicians involved to become aware of the different clinical spectrums with which SLE can present.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient consent is not required as patient identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-Assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- 2019 EULAR/ACR classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71:1400-12.
- [CrossRef] [PubMed] [Google Scholar]
- A practical perspective of the hematologic manifestations of systemic lupus erythematosus. Cureus. 2022;14:e22938.
- [CrossRef] [Google Scholar]
- Pediatric systemic lupus erythematosus with lupus anticoagulant hypoprothrombinemia syndrome-A case series with review of literature. Lupus. 2021;30:641-8.
- [CrossRef] [PubMed] [Google Scholar]
- Warm autoimmune hemolytic anemia as the initial presentation of systemic lupus erythematosus (SLE): A case report. Am J Case Rep. 2021;22:e932965.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral branch retinal artery occlusion in a patient with systemic lupus erythematosus: A case report. Medicine (Baltimore). 2022;101:e29005.
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychiatric involvement in juvenile-onset systemic lupus erythematosus: Data from the UK Juvenile-onset systemic lupus erythematosus cohort study. Lupus. 2021;30:1955-65.
- [CrossRef] [PubMed] [Google Scholar]
- SLE initially presenting with neuropsychiatric manifestations and seizure, a case report. Immun Inflamm Dis. 2023;11:e918.
- [CrossRef] [PubMed] [Google Scholar]






