Translate this page into:
Continuous versus intermittent mask use by nurses in COVID times (CIMNIC) – A CUSUM study
*Corresponding author: Neeraj Gupta, Department of Pediatrics, Sir Gangaram Hospital, New Delhi, India. drneeraj1979@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta N, Agarwal P, Sachdev A, Gupta S, Gupta D, Rajan S, et al. Continuous versus intermittent mask use by nurses in COVID times (CIMNIC) – A CUSUM study. Karnataka Paediatr J 2022;37:79-85.
Abstract
Objectives:
The coronavirus disease 2019 pandemic has reinforced the use of personal protective equipments in healthcare settings. Although filtering face piece 2 respirators provide adequate protection from the aerosolised viral spread, their prolonged use is often associated with subjective discomfort. The study aimed to identify whether an intervening mask-free period is less harmful in terms of discomfort and desaturation when compared against continuous use for 6-h.
Material and Methods:
This was a prospective and interventional study. A cohort of 87 previously healthy nurses from a multidisciplinary tertiary care hospital were recruited. Study participants were subjected to continuous and intermittent (with 15 min break) mask use, each for a 2-month duration, during their 6-h clinical shifts. Baseline and post-shift oxygen saturation (SpO2) were compared in real time using cumulative sum (CUSUM) statistics. Comfort level was also assessed on a scale of 0–10 in the two groups with 10 subjective parameters.
Results:
Nurses have experienced a significant drop in SpO2 in both phases with 525 and 984 recordings in continuous and intermittent mask group, respectively. The mean % (2SD) saturation drop in the two groups was 4.688 (39.35) and 1.169 (2.62). The overall discomfort level was more in the continuous phase (8.89 ± 1.610) than in intermittent (7.28 ± 3.216) mask use. CUSUM statistics helped in the real-time monitoring of subjects in the intermittent mask group.
Conclusions:
Significant adverse health effects in healthcare workers are highlighted using objective and subjective parameters such as desaturation and discomfort levels while using protective face masks. A mask-free period of 15 min, in between their duty shifts, might help reduce the unfavourable effects without compromising efficacy.
Keywords
Coronavirus disease
Nurses
Cumulative sum
Oxygen saturation
Comfort score
INTRODUCTION
Coronavirus disease 2019 (COVID-19), the latest pandemic witnessed by the current generation, started at a small place in Wuhan, China in December 2019 and later became a global health crisis within a short period.[1,2] By February 23, 2022, the disease had already affected approximately 425 million people across the world with nearly 6 million deaths and numbers still counting.[3] The high infectivity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the pathogen responsible for the COVID-19 outbreak, has been attributed to its airborne transmission.[4] The tiny, 0.06–0.12 µ SARS-CoV-2 virus, spreads through either droplet (>5 µ) during coughing and sneezing or aerosol (<5 µ) production during loud speaking and even in quiet breathing.[5] Aerosol-generating procedures such as intubation, positive pressure ventilation, bronchoscopy, upper gastrointestinal endoscopy, airway toileting and dental extraction are common in healthcare settings which put healthcare workers at significantly higher risk of contracting the disease than the general population.[6] N-95 face masks or equivalent filtering face piece 2 (FFP2) respirators, which can filter up till 95% of 0.3-micron and larger particles usually, provide adequate protection against airborne COVID-19 transmission by trapping the coronavirus due to its rapid brownian motion.[7] Hence, the World Health Organization and Centers for Disease Control and Prevention have universally recommended N-95 face masks or FFP2 respirators for healthcare providers, as a part of personal protective equipment (PPEs), while dealing with high-risk patients for COVID-19 transmission.[3,7]
Recently, serious concerns have been raised regarding the safety of these protective face masks, especially by healthcare providers. People have complained of suffocation, breathlessness, sweating, and feeling of discomfort after using them for a prolonged period.[8-10] This led to hindrance on part of users to follow recommended preventive practices adequately and predisposing them to increased risk of cross-infections.[11] Arora and colleagues have highlighted the unmet need to address various practical issues with the use of PPEs to minimise infection spread.[12] Few alternatives have been tried to improve the safety while retaining the efficacy of facemasks such as nano-treatment and various other types of surgical masks but with limited benefits.[8,13] Sickbert-Bennett et al. tried using a surgical face mask to improve user acceptance but found objectionable efficacy.[14] None of the surrogate strategies have been an ideal replacement for conventional respirators till date. Therefore, we planned to conduct this CIMNIC study to compare the safety profile of respirators in nurses, during their continuous or intermittent use, in real-time using cumulative sum (CUSUM) and conventional statistics.
MATERIAL AND METHODS
Trial oversight
This prospective and interventional study was conducted at a 675-bedded multispecialty tertiary care referral hospital of North India. Institutional review board approval was obtained before the enrolment of subjects (EC/01/21/1584).
Study subjects
Previously healthy nurses, who were working in hospital non-COVID clinical areas, were enrolled in the study after taking their informed consent to participate.
Procedures
The study was conducted on the same cohort of nurses in two phases, each for a consecutive 2 months duration, for the assessment of oxygen saturation (SpO2) and comfort score after using an FFP2 face mask (3M 9504-IN Respirator) by the nurses. In the first phase, the face mask was worn continuously during their 6-h duty shift (standard of care as per hospital protocol). In the second phase, a 15-min mask-free period was allowed in between 2.5 and 3.5 h of their shifts. During the mask-free period, nurses were allowed to rest in room air in a well-ventilated separate room either individually or with appropriate social distancing. SpO2 readings were recorded by using a Contec CMS-70A pulse oximeter at the start and again at the completion of their duty shifts, just before removal of FFP2 mask. All measurements were noted in resting sitting position during quiet breathing for 60 s at 25°C room temperature in the right index finger of nurses.[15] The most stable SpO2 value with strong pulse signal was recorded for the purpose of study. No recordings were done in presence of nail polish, wet, or cold hands. All SpO2 readings were recorded by one among the group of four trained technicians, after a 2-h training session at the start of study, by the paediatric intensivist. Post-shift saturations were compared against the baseline in both groups. Saturation change in continuous group was used as standard parameters for CUSUM statistics, against which findings in intermittent group were compared in real-time per subject. A modified comfort scale (with addition of nose pain and headache in the comfort scale used by Li et al.) was used to monitor comfort level of nurses after face-mask use at the end of their duty shifts each time [Supplemental Material].[8,16] Nurses were asked to record their subjective perception (on a scale of 10 with score of 0 for nil and score of 10 for maximum) regarding various parameters such as humid, hot, breath resistance, itchy, tight, salty, smelly, body fatigue, nose pain and headache. Overall discomfort was also quantified individually in both groups.
Outcome measures
Change in post-shift SpO2 as compared to baseline and subjective comfort parameters was measured during both phases of study.
Statistical analysis
A 3% or more drop in SpO2 from baseline was considered as failure whereas rest of recordings were considered successful for the purpose of the present study.[17] The SpO2 data were arranged as either success (S) or failure (F) in the continuous mask use group and fed in the previously validated CUSUM software (available at https://jacob.puliyel.com/foresee/).[18] Using the boot strapping method with 10,000 iterations, upper and lower CUSUM control lines were created by the available software, which corresponded to mean upper CUSUM score + 2SD and mean lower CUSUM score −2SD, respectively. The weightage of each S and F was calculated, by the software, such that the total sum of whole data came zero. SpO2 differences from the baseline in intermittent mask group were categorised as either S and F, using the same weightage as calculated previously, and fed simultaneously in CUSUM calculator. Success and failure in the intermittent group were monitored in real-time graphic pattern. We have also applied conventional statistics on the study parameters (mean change in SpO2 and comfort score) in two groups. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) programme for Windows, version 17.0 (SPSS, Chicago, Illinois). Continuous variables are presented as mean ± SD and categorical variables are presented as absolute numbers and percentage. Normally distributed continuous variables were compared using the unpaired t-test. Categorical variables were analysed using either the Chi-square test or Fisher’s exact test. Paired test was used for comparison of continuous variables from preand post-intervention. P < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
Eighty-seven nurses, between 20 and 44 years of age, participated in the study. During the initial 2 months of the study period with continuous 6-h face mask use, 559 readings were recorded. After excluding 34 readings (due to either incomplete data or nail polish use), 525 readings were subjected to final analysis. During the next 2 months of intermittent face mask use, 1009 readings from the same nurses’ group were recorded, out of which 984 were included in the final analysis.
Outcomes
The mean baseline SpO2 in the two study groups was similar, while post-shift saturations were significantly different [Table 1]. There was a marked drop in (mean ± 2SD) SpO2 values in the continuous group as compared to the intermittent group (4.688 ± 39.351 vs. 1.169 ± 2.626) after using the FFP2 respirator. There were 296 (n-525) recordings of ≥a 3% drop in SpO2 after continuous mask use as compared to only 291 (n-984) in the intermittent mask use phase. The weightage for each success and failure was + 1.127 and −0.872, respectively. The upper and lower CUSUM control lines were plotted at CUSUM scores of +28.59 and −28.93, respectively, using data from the continuous mask group. The real-time CUSUM plot for intermittent mask use crossed the upper control line within the initial 30 readings [Figure 1] and thereafter always remained above the upper CUSUM control line [Figure 2]. The subjective comfort score parameters were appreciably more affected in the continuous group as compared to others [Table 1 and Figure 3]. Overall (the mean ± 2SD) discomfort level was significantly less in nurses when they were provided a 15-min mask-free period in between their shifts (7.28 ± 3.216 vs. 8.89 ± 1.610 in the intermittent and continuous group, respectively).
| Parameter | Continuous group | Intermittent group | P value |
|---|---|---|---|
| Number of observations (n) | 525 | 984 | |
| Female: Male | 520:5 | 983:1 | |
| Mean±SD | |||
| Age (in years) | 30.34±4.477 | 33.17±12.506 | |
| % Oxygen saturation (SpO2) | 0.264 | ||
| Baseline | 99.48±39.302 | 97.56±2.188 | <0.001 |
| Post-shift | 94.79±1.972 | 96.39±1.507 | 0.007 |
| ∆SpO2 | 4.688±39.351 | 1.169±2.626 | <0.001 |
| Post shift subjective scores (on a scale of 10) | |||
| Humid | 8.31±2.059 | 6.49±2.953 | <0.001 |
| Hot | 8.49±1.910 | 6.56±3.100 | <0.001 |
| Breath resistance | 8.28±1.773 | 6.48±2.869 | <0.001 |
| Itchy | 7.63±2.474 | 6.10±3.240 | 0.001 |
| Tight | 8.17±2.364 | 6.59±3.201 | <0.001 |
| Salty | 6.93±3.402 | 5.82±3.718 | 0.041 |
| Smelly | 7.40±2.939 | 6.22±3.411 | 0.015 |
| Body fatigue | 8.18±2.165 | 6.83±3.122 | 0.001 |
| Nose pain | 8.56±1.847 | 7.56±2.896 | 0.007 |
| Headache | 8.55±1.909 | 6.98±3.217 | <0.001 |
| Overall discomfort | 8.89±1.610 | 7.28±3.216 | <0.001 |

- Cumulative sum graph with the two control lines and initial data from the intermittent mask use group.
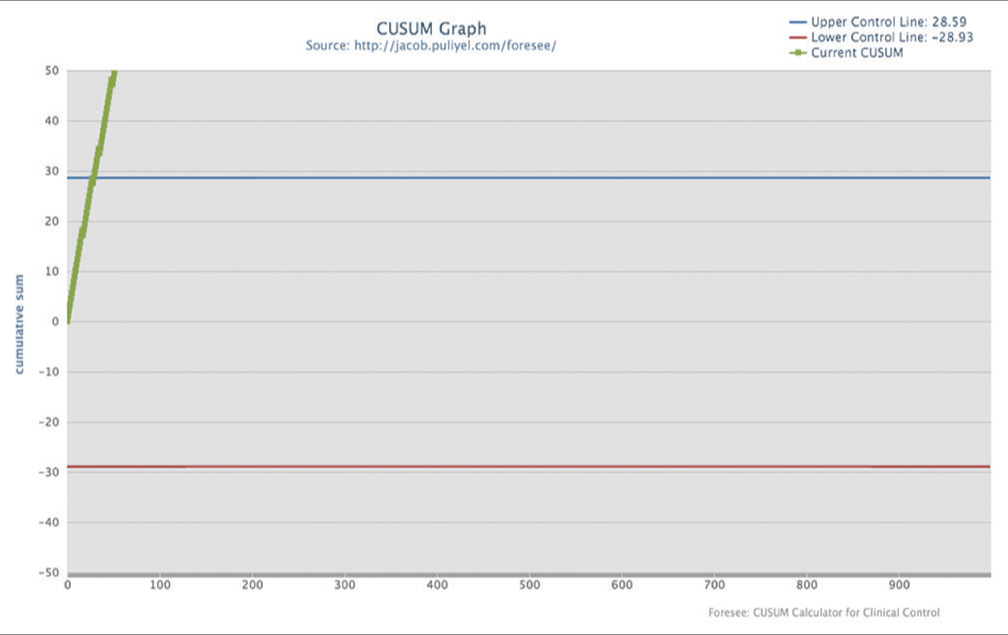
- Cumulative sum graph for the complete data of intermittent mask use group.
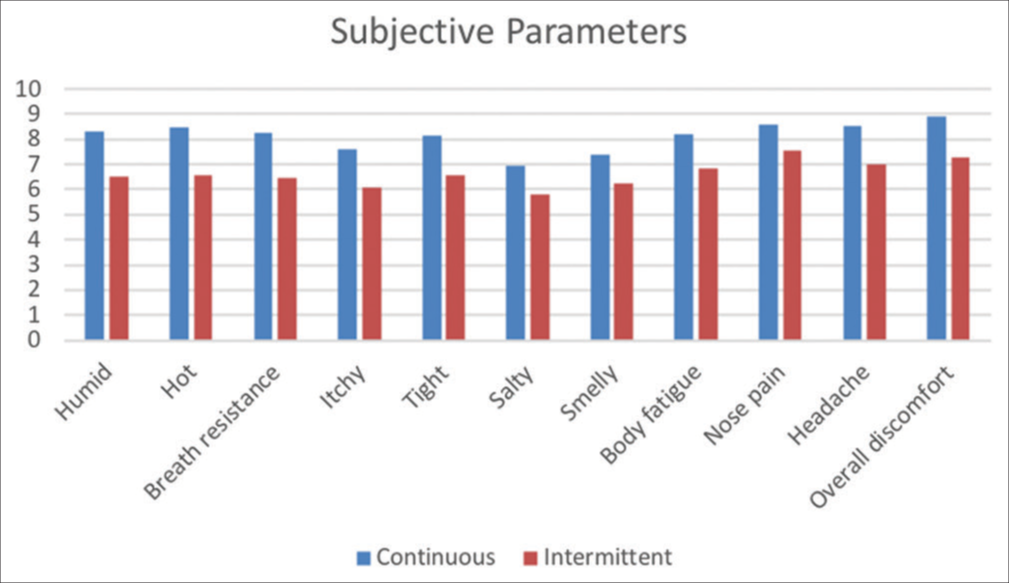
- Comparison of subjective scores on a scale of 10 in the study groups.
DISCUSSION
The standard of care FFP2 respirators (N-95 mask) are associated with physical and subjective discomfort when used for a protracted duration. Breathing difficulties and tiredness are common findings along with headache and local pain as reported previously. The number of analysable recordings in the two phases was 525 and 984, respectively, in our study. This difference can be explained by a varied number of shifts by nurses as per the hospital policies. The mean age of participants in the two time sets were 30.34 and 33.17 years, which is due to the different quantum of work by the same nurse’s cohort [Table 1].
The mean baseline SpO2 in the two groups were similar; however, there was a significant drop in SpO2 by 4.688% in the continuous mask group as compared to less than one-third drop in the intermittent group. Nurses have experienced a significant downward SpO2 trend during routine clinical duties in both groups. As per the British Thoracic Society guidelines for oxygen use, a drop in SpO2 of 3% or more from baseline may indicate an alarming situation even if SpO2 is >94% in a healthy person, which warrants further evaluation.[17] This translates to an enormous risk of hypoxemia in healthcare workers who are using respirators continuously.
CUSUM is a statistical technique used commonly in industries for quality control assessment. After assigning positive and negative weights for previously defined successes (S) and failures (F) from a standard process, the original sequence of S and F is randomly reordered 10,000 times using the bootstrapping method.[18] The highest and lowest limits of CUSUM are defined for each iteration, that can occur by chance, and thereafter upper CUSUM control line (mean upper CUSUM + 2SD) and lower CUSUM control line (mean lower CUSUM – 2SD) are drawn using data from all the iterations.[18] Gupta et al. have derived, validated and patented a CUSUM software for easy weightage calculations, boot strapping and for drawing control lines.[19] S and F from any new intervention can be plotted in real time to compare it against the standard of care. If the real-time graph remains in between two CUSUM control lines, then the new intervention is not considered statistically distinct from the standard one. On the other hand, if the graph crosses any CUSUM control line then there is significant difference between the two interventions. Puliyel and Puliyel have earlier used this technique for competency monitoring of trainees during cataract extraction.[18]
CUSUM has been used earlier by Gupta et al. to identify the effect of nebulised hypertonic-saline against epinephrine in children with bronchiolitis.[19] Kinsey et al. assessed antimicrobial treatment in neutropenic patients using this technique.[20] Ravn et al. have evaluated clinical competence of medical trainees using CUSUM analysis.[21] Fortea-Sanchis et al. used CUSUM charts to assess the nodal analysis quality in colon cancer.[22] This statistical tool has a distinct advantage over others, in terms of real time monitoring of experimental trial. Any potentially harmful process can be immediately stopped if the graph crosses the lower CUSUM control line at any point of time in between the study. We have used CUSUM statistics to highlight the importance of mask-free period in prevention of significant hypoxemia in healthcare workers. The healthcare workers experienced significantly less desaturations during the intermittent mask use phase as compared to standard of care.
Researchers have evaluated subjective discomfort in people using respirators. Dugdale and Walensky found N-95 masks as suffocating, uncomfortable and intolerable when used for prolonged duration.[23] Li et al. have demonstrated that people using N-95 mask experienced higher heart rates, more temperature and humidity as compared to surgical facemask during their study in 10 healthy subjects who were subjected to treadmill exercise.[8] Locatelli et al. highlighted discomfort and skin irritation experienced by healthcare workers using FFP mask.[16] Zhu et al. have found increased mean nasal resistance and discomfort level with increasing duration of N-95 mask use in their work on 87 healthcare workers.[9] Farronato et al. in their survey including 256 dentists found strong association of headache, discomfort and impaired work ability with prolonged respirator use.[6] Rosner in their cross-sectional study among 343 health-care professionals found that prolonged use of facemask causes headache, rash, skin breakdown and impaired cognition.[24] Purushothaman et al. have highlighted significant discomfort in 250 healthcare workers while wearing facemask for prolonged duration, in their questionnaire based study.[10] We have also found significant adverse subjective feelings in participants for all 10 study parameters with mean discomfort level of 8.89 and 7.28, on a scale of 0–10, in two different time periods [Table 1]. Prolonged intermittent hypoxia and discomfort level will potentially cause personal health hazard and professional dissatisfaction in users.
There have been active search for safe and effective alternatives to N-95 mask/FFP2 respirators. Zhu et al. have found less increase in nasal resistance and associated discomfort in healthcare employees with use of surgical facemask as compared to N-95 mask.[9] Shenal have studied various types of respiratory protection in health-care settings and concluded highest level of discomfort while using N-95 and medical mask combination followed closely by N-95 masks when used alone.[13] They observed that the powered air-purifying respirators were associated with minimal discomfort which was still significant with prolonged duration of use. After careful literature search, we were unable to find any widely acceptable cost-effective interventions, which can be utilised in resource poor countries, to improve the safety of existing face masks while retaining their efficacy. In our study, there was a significant improvement in comfort level of nurses with the introduction of 15 min break in between their 6 h duty shift [Table 1]. Intermittent use of respirators might be less harmful than their continuous use in healthcare workers while retaining their protective efficacies.
Limitations of the study
Although there is a theoretical possibility of bias about the responses during the second phase of study as similar group of nurses was interviewed in both phases, but this risk seems negligible as comfort scores were assessed in different time periods and mainly depended on short-term memory recall. We have not evaluated the correlation of degree of hypoxemia and subjective discomfort in various domains. A multicentric study with inclusion of more parameters such as assessment of carbon-dioxide retention, effect on quality of life and long-term neurocognitive outcomes in healthcare workers needs to be planned in future.
CONCLUSION
CIMNIC study provides an applicable insight to important health aspects of care takers while using protective face masks. An intervening mask free period at periodic intervals is warranted as one of the preventive health strategy for healthcare workers. CUSUM methodology was quiet useful to monitor the effects of intermittent mask use in real-time.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
KEY MESSAGES
Health-care providers are subjected to significant discomfort and hypoxemia during their routine clinical work during COVID-19 pandemic. A simple strategy like short mask free interval can be helpful to reduce the long-term adverse consequences of prolonged usage, without compromising efficacy.
IMPLICATIONS FOR CLINICAL PRACTICE
Prolonged surgical masks wearing, during long-term shifts of nurses and other healthcare workers are harmful in terms of subjective discomfort and objective drop in oxygenation. Long-term adverse effects, on both physical and mental health, of such transient harms needs to be studied with prospective and long-term studies. Harms can be significantly reduced by simple strategies like intermittent short-term mask free period. The present study widens the scope of CUSUM statistics use for real-time monitoring of new interventions in the health-care settings.
SUPPLEMENTAL MATERIAL

- CIMNIC study - Comfort score
Financial support and sponsorship
Nil.
References
- Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565-74.
- [CrossRef] [PubMed] [Google Scholar]
- Advice on the Use of Masks in the Community. Available from: https://www.who.int/docs/default-source/documents/advice-on-the-use-of-masks-2019-ncov.pdf [Last accessed on 2021 Jan 22]
- [Google Scholar]
- Coronavirus Disease (COVID-19) Outbreak Situation. 2022. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Last accessed on 2022 Feb 23]
- [Google Scholar]
- Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564-7.
- [CrossRef] [PubMed] [Google Scholar]
- Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382:872-4.
- [CrossRef] [PubMed] [Google Scholar]
- A scoping review of respirator literature and a survey among dental professionals. Int J Environ Res Public Health. 2020;17:5968.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus (COVID-19) Available from: https://www.cdc.gov/coronavirus/2019-ncov/index.html [Last accessed on Jul 02]
- [Google Scholar]
- Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Arch Occup Environ Health. 2005;78:501-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of long-duration wearing of N95 respirator and surgical facemask: A pilot study. J Lung Pulm Respir Res. 2014;1:97-100.
- [CrossRef] [Google Scholar]
- Effects of prolonged use of facemask on healthcare workers in tertiary care hospital during COVID-19 pandemic. Indian J Otolaryngol Head Neck Surg. 2020;73:59-65.
- [CrossRef] [PubMed] [Google Scholar]
- Are health care workers following preventive practices in the COVID-19 pandemic properly?-A cross-sectional survey from India. Diabetes Metab Syndr. 2020;15:69-75.
- [CrossRef] [PubMed] [Google Scholar]
- Real-world assessment, relevance, and problems in use of personal protective equipment in clinical dermatology practice in a COVID referral tertiary hospital. J Cosmet Dermatol. 2020;19:3189-98.
- [CrossRef] [PubMed] [Google Scholar]
- Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg. 2012;9:59-64.
- [CrossRef] [PubMed] [Google Scholar]
- Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Intern Med. 2020;180:1607-12.
- [CrossRef] [PubMed] [Google Scholar]
- Pulse oximetry for monitoring patients with COVID-19 at home. Potential pitfalls and practical guidance. Ann Am Thorac Soc. 2020;17:1040-6.
- [CrossRef] [PubMed] [Google Scholar]
- Health care workers' reported discomfort while wearing filtering face-piece respirators. Workplace Health Saf. 2014;62:362-8.
- [CrossRef] [PubMed] [Google Scholar]
- BTS Emergency Oxygen Guideline Development Group, BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. 2017;72:ii1-90.
- [CrossRef] [PubMed] [Google Scholar]
- CUSUM for monitoring competency: Computer software is useful for bootstrapping and real-time CUSUM plotting. Br J Ophthalmol. 2011;95:295-6.
- [CrossRef] [PubMed] [Google Scholar]
- Nebulized hypertonic-saline vs epinephrine for bronchiolitis; proof of concept study of cumulative sum (CUSUM) analysis. Indian Pediatr. 2012;49:543-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cusum plotting of temperature charts for assessing antimicrobial treatment in neutropenic patients. BMJ. 1989;299:775-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cusum-score. The cusum score. A tool for evaluation of clinical competence. Ugeskr Laeger. 2001;163:3644-8.
- [Google Scholar]
- CUSUM charts in the quality control of colon cancer lymph node analysis: A population-registry study. World J Surg Oncol. 2018;16:230.
- [CrossRef] [PubMed] [Google Scholar]
- Filtration efficiency, effectiveness, and availability of N95 face masks for COVID-19 prevention. JAMA Intern Med. 2020;180:1612-3.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. 2020;6:130.
- [CrossRef] [Google Scholar]






