Translate this page into:
Emergent challenges in paediatric tracheostomy care: Insights from a case report
*Corresponding author: Anurag V. Kumar, Department of Pediatrics, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. anuragvkumar123@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Surendran AK, Vishak MS, Kumar AV. Emergent challenges in paediatric tracheostomy care: Insights from a case report. Karnataka Paediatr J. 2024;39:106-9. doi: 10.25259/KPJ_18_2024
Abstract
Tracheostomy is a common surgical procedure in paediatric patients that can lead to life-threatening complications such as tube breakage. This case report highlights the management of tracheostomy tube breakage in a 3-year-old male with Down’s syndrome and subglottic stenosis. On presentation with cough and cyanosis, the patient was found with a missing tracheostomy tube, leading to prompt intervention. Imaging revealed a broken tube in the left main bronchus, prompting successful extraction under general anaesthesia. The case underscores the importance of timely action and multidisciplinary care in such emergencies. The literature review reveals sparse discussion on paediatric tracheostomy tube breakage, emphasising the need for increased awareness and preventative measures. This report contributes to understanding and managing this uncommon yet critical complication, emphasising the necessity of thorough inspection and adherence to quality standards to ensure patient safety.
Keywords
Tracheostomy
Stenosis
Extubation
Emergencies
X-ray
INTRODUCTION
Tracheostomy is a surgical procedure in which an opening is created in the anterior trachea to facilitate respiration. Indications of tracheostomy include subglottic stenosis, ventilator dependence for a prolonged period, refractory obstructive sleep apnoea, and chronic aspiration, to mention a few. Complications such as accidental decannulation, obstruction, and haemorrhage are life-threatening, while tracheal stenosis, infections, and tracheocutaneous fistula formation are the minor ones, with a total occurrence rate of >50%.[1] Tracheostomy-related emergencies, if not managed properly, lead to significant morbidity and mortality, with the 30-day mortality being high, emphasising the need for multidisciplinary evaluation and a well-prepared emergency care provider.[2]
Paediatric tracheostomy rates have decreased over the years, but the complications have become more severe. Early wound identification protocols, reducing prolonged pressure, and skin care methods have helped significantly reduce the incidence and impact of these complications.[3] Tracheostomy tube breakage, though rare, is a dangerous complication, especially in the paediatric age group, as the broken tube needs to be taken out while maintaining the airway patency adequate for ventilation. Fragmented and migrated tracheostomy tubes have been reported as a life-threatening complication by Al-Momani et al. in the literature.[4] Corrosion and breakage of metal tracheostomy tubes have also been reported, imposing strict regulations over production control and quality.[5]
We present to you a case report with tracheostomy tube breakage in the paediatric age group, with the primary objective being the fact that such an emergency requires prompt action, along with highlighting ways to manage them. We hope to enhance our understanding of this emergency and its treatment by presenting the case and reviewing prior studies. Through this rare case study, we aim to provide readers with a better knowledge of tracheostomy tube breakage, which will make it easier for medical practitioners to identify and treat patients presenting with such a complication.
CASE REPORT
The patient is a 3-year-old male child a known case of Down’s syndrome and subglottic stenosis (tracheostomy done at day 65 of life), who presented to the paediatric casualty with increased cough and bluish discoloration of the face. The child had decreased alertness, and the tracheostomy tube was missing, with only the flange intact. The child’s vitals were a pulse rate of 128/min, blood pressure of 90/52 mmHg, respiratory rate of 48/min, and the child was afebrile. There was no history of seizures, fever, or any other complaints. Physical examination revealed reduced air entry to the left lung. The rest of the systemic examination was normal.
Past history was significant for transient myeloproliferative disorder for 2 years, which had been managed effectively with multiple platelet transfusions, leading to resolution. Karyotyping revealed the Trisomy of chromosome 21. In addition, the patient had severe tricuspid regurgitation suggestive of pulmonary arterial hypertension, for which sildenafil and inotropes were administered. Subsequent echocardiography indicated normalisation at 2 months. Furthermore, the patient experienced a year back, right upper lobe pneumonia, which was successfully treated with sulbactam/cefoperazone and amikacin over a 10-day period. Due to repeated extubation failures, the child underwent a tracheostomy at 65 days of life. On-going ENT follow-ups advised tube changes every 15 days, with the last change performed at home 10 days prior.
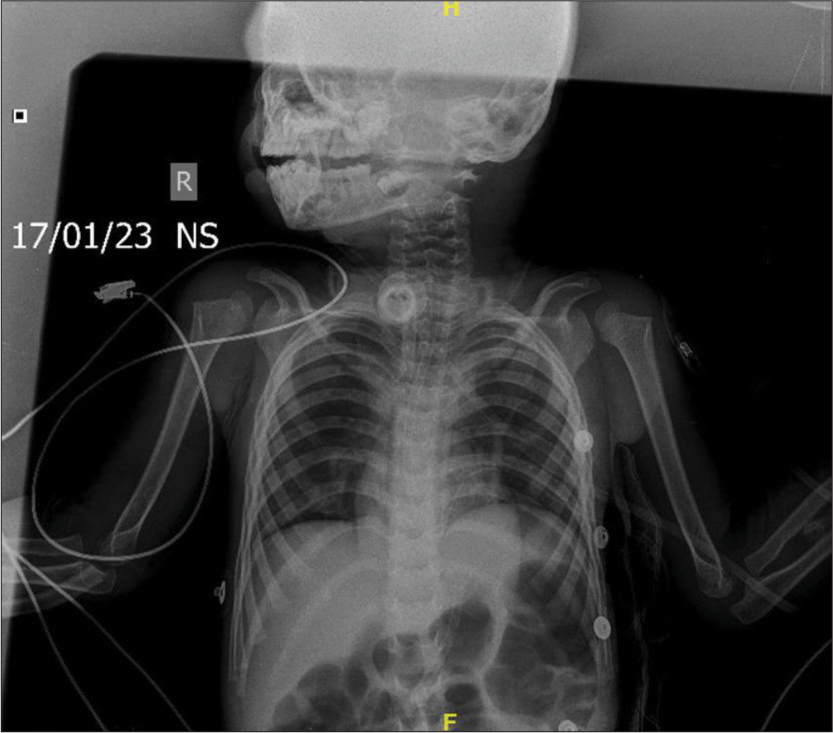
On admission, the child was supported by bag and tube ventilation while maintaining satisfactory saturation with 5L O2 through T piece. Subsequently, subcutaneous emphysema was observed on the left chest wall along with pneumothorax. A chest X-ray revealed a broken tracheostomy tube in the left main bronchus area [Figure 1], prompting an ENT consultation for foreign body removal. Under general anaesthesia, the skin stoma was revised, enabling visualisation of the tracheostomy tube. Using optical forceps and a telescope introduced through the tracheostomy, the broken tube in the left bronchus was successfully extracted and replaced with a size 4 cuffed tracheostomy tube [Figure 2]. Haemostasis was achieved, and the child was then transferred back to the paediatric intensive care unit. Post-procedure, the child’s condition remained stable, with resolved pneumothorax and persistent subcutaneous emphysema. Due to borderline saturation levels (89–91%), the child was initiated on 2 L/min O2 through T piece. Suture removal was done on the 7th day, and ENT follow-up was advised.

- X-ray showing broken tracheostomy tube in the left main bronchus (Blue arrow).
- X-ray taken after removal of the broken tracheostomy tube.
DISCUSSION
In critically ill patients who require extended mechanical ventilation for acute respiratory failure and airway problems, tracheostomy is a routinely done intervention. With an average of over 100,000 tracheostomies being performed every year,[6] the complications that arise out of the procedure require prompt management to avert life-threatening crises or significant morbidity. While tracheostomy is considered a life-saving treatment in certain clinical scenarios – the paediatric population is still at a higher risk than adults. The increased survival rates among premature newborns and those born with severe congenital disabilities, however, have led to a dramatic change in the rationale for tracheostomy in paediatric patients over the past few decades.
Being a life-saving intervention often employed in pediatric patients with complex medical conditions, for essential respiratory support and management, tracheostomy-related emergencies can be very difficult to handle unless recognised and managed urgently. Tracheostomy tube breakage has been reported in the literature[4,5,7] in which a broken tube in a 4.5-year-old child was removed after imaging using rigid bronchoscopy in the first case. Kock et al.[5] focused more on the need for strict regulation practices during the production of tracheostomy tubes, while Erdozáin Rodríguez et al.[7] reported the aspiration of the inner cannula into the left tracheobronchial tree and is one of the earliest reported cases of tracheostomy tube breakage.[4] Krishnamurthy and Vijayalakshmi reported right main bronchus and trachea are the most common sites for the dislodged components of a broken tracheostomy tube being trapped.[8] The common approach of removal of the broken parts through rigid bronchoscopy was done by Atwood et al. in a case where the tube broke at the junction of the cannula and neck plate.[9]
Tracheal polyps causing rupture of the tracheostomy tube cuff have also been reported in a rare case by Feifei et al.[10] Tracheobronchopathia osteochondroplastica, a rare benign disorder of the bronchi and trachea, was also reported to cause cuff rupture. Wilson et al., in a case similar to the one reported by Erdozáin Rodríguez et al., reported that the aspirated foreign body was removed by flexible bronchoscopy.[7,11] Studies have well addressed, how to prevent tracheostomy tube breakage. In one case, Loh et al. recommended regular follow-up and tube replacement.[12] In another case involving a 14-year-old child, Piromchai et al. suggested that proper cleaning and following a schedule for tube changes can help prevent breakage and associated complications.[13]
Breakage is caused by a number of causes, including manufacturing flaws, repeated handling, and exposure to specific cleaning agents – which can cause the tracheostomy tube to fragment and migrate. The available literature highlights the importance of early detection and treatment in general, as patients are immediately at risk from foreign body aspiration.
Paediatric tracheostomy tube breakage and its management have not been discussed much before in literature.
Prompt and effective treatment is crucial to avoid life-threatening situations from rare but dangerous tracheostomy tube breakage in young patients. This case, involving a child with Down’s syndrome and subglottic stenosis, exemplifies the unique challenges of managing such a break. Through this article, we have explored the strategies and difficulties associated with the management of this paediatric emergency.
Reviews of the literature highlight the importance of careful inspection and quality checks prior to the initial use of tracheostomy tubes, particularly in situations where inner cannulas may be prone to fracture. These incidents highlight the necessity of thorough preventative measures to avoid tracheostomy tube breaking, which include careful examination for manufacturing flaws, adherence to correct handling procedures, and routine inspection for potential corrosion in metal tubes. Such preventative measures are necessary to guarantee the security and welfare of patients who depend on tracheostomies for breathing support.
CONCLUSION
Paediatric tracheostomy tube breakage is a serious though not a well-reported area in scientific literature. Through this case report, we aim to provide insightful information about the efficient management and preventative measures essential in ensuring the well-being of paediatric patients with tracheostomies by critically analysing the cases and situating them within the larger framework of paediatric tracheostomy care.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tracheostomy emergencies. Emerg Med Clin North Am. 2019;37:109-19.
- [CrossRef] [PubMed] [Google Scholar]
- Retrospective analysis of post-tracheostomy complications. Am J Otolaryngol. 2022;43:103350.
- [CrossRef] [PubMed] [Google Scholar]
- Managing complications of percutaneous tracheostomy and gastrostomy. J Thorac Dis. 2021;13:5314-30.
- [CrossRef] [PubMed] [Google Scholar]
- Upper airway obstruction by a fragmented tracheostomy tube: Case report and review of the literature. Int J Surg Case Rep. 2015;17:146-7.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate postoperative complications in adult tracheostomy. Cureus. 2020;12:e12228.
- [CrossRef] [Google Scholar]
- Tracheobronchial foreign body in the laryngectomized patient. An Otorrinolaringol Ibero Am. 1998;25:185-92.
- [Google Scholar]
- Broken tracheostomy tube: A fractured mandate. J Emerg Trauma Shock. 2012;5:97-9.
- [CrossRef] [PubMed] [Google Scholar]
- A fractured tracheostomy tube causing airway compromise. Am J Case Rep. 2022;23:e936072.
- [CrossRef] [PubMed] [Google Scholar]
- Nursing care of patient with tracheostomy tube cuff rupture caused by tracheal polyp: A case report. Crit Care Nurse. 2023;43:52-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture and aspiration of tracheostomy tube: A case report. Hong Kong J Emerg Med. 2018;25:371-3.
- [CrossRef] [Google Scholar]
- Fracture and aspiration of a tracheostomy tube. BMJ Case Rep. 2014;2014:bcr2013203232.
- [CrossRef] [PubMed] [Google Scholar]
- Fractured metallic tracheostomy tube in a child: A case report and review of the literature. J Med Case Reports. 2010;4:234.
- [CrossRef] [PubMed] [Google Scholar]







