Translate this page into:
Gastric perforation: A devastating surgical emergency in a preterm neonate with multidrug-resistant Klebsiella pneumoniae sepsis – A case report
*Corresponding author: H. A. Venkatesh, Department of Neonatology, Manipal Hospital, Bengaluru, Karnataka, India. venkatveena46@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Venkatesh HA, Reddy AS, Venkatesh S. Gastric perforation: A devastating surgical emergency in a preterm neonate with multidrug-resistant Klebsiella pneumoniae sepsis – A case report. Karnataka Paediatr J. doi: 10.25259/KPJ_60_2024
Abstract
A preterm twin neonate with Klebsiella pneumoniae developed free gas within the peritoneal cavity on D3 of life due to gastric perforation. Gastric perforation in neonates, especially preterm neonates, is a devastating surgical emergency and it is a major challenge for the treating physician with a mortality rate of 30–50%. It was first reported by Siebold. Many etiologies including ischemia, aerophagy, trauma, absent muscular layer and sepsis are considered. Whatever the etiology the intervention is needed urgently to prevent mortality and morbidity. We present a preterm neonate with multidrug-resistant K. pneumoniae who developed sudden abdominal distension needing exploration and repair of gastric perforation. Despite being managed by early resuscitation and stabilisation with surgical repair of the defect, he succumbed to illness post-surgery.
Keywords
Gastric perforation
Mortality
Preterm
Sepsis
INTRODUCTION
Gut perforation is an important clinical morbidity in preterm and neonates. Spontaneous intestinal perforation or secondary to necrotizing enterocolitis is one of the reasons for the perforation. A preterm neonate on medication containing indomethacin and hydrocortisone has more chance of gut perforation. Timely recognition and management can reduce mortality and morbidity. Sepsis is an added disadvantage in preterm neonates with sepsis having a high mortality rate.
CASE REPORT
We report a case of a premature male infant born at 32 weeks of twin gestation to a mother conceived by in vitro fertilisation by elective C-section. He developed sudden abdominal distension on d3 of life and was less active [Figure 1a]. Mother had premature rupture of membrane for 48 h before the delivery with no additional information of significance. At birth he cried immediately after birth and needed continuous positive airway pressure (CPAP) support. He was shifted to the neonatal intensive care unit and connected to a ventilator CPAP. He required minimal oxygen support to maintain adequate saturation. He was started on donor human milk at 12 h of age and his vitals remained stable. He was started on intravenous ampicillin and gentamycin due to preterm premature rupture of the membrane. He passed stools and continued to be active.
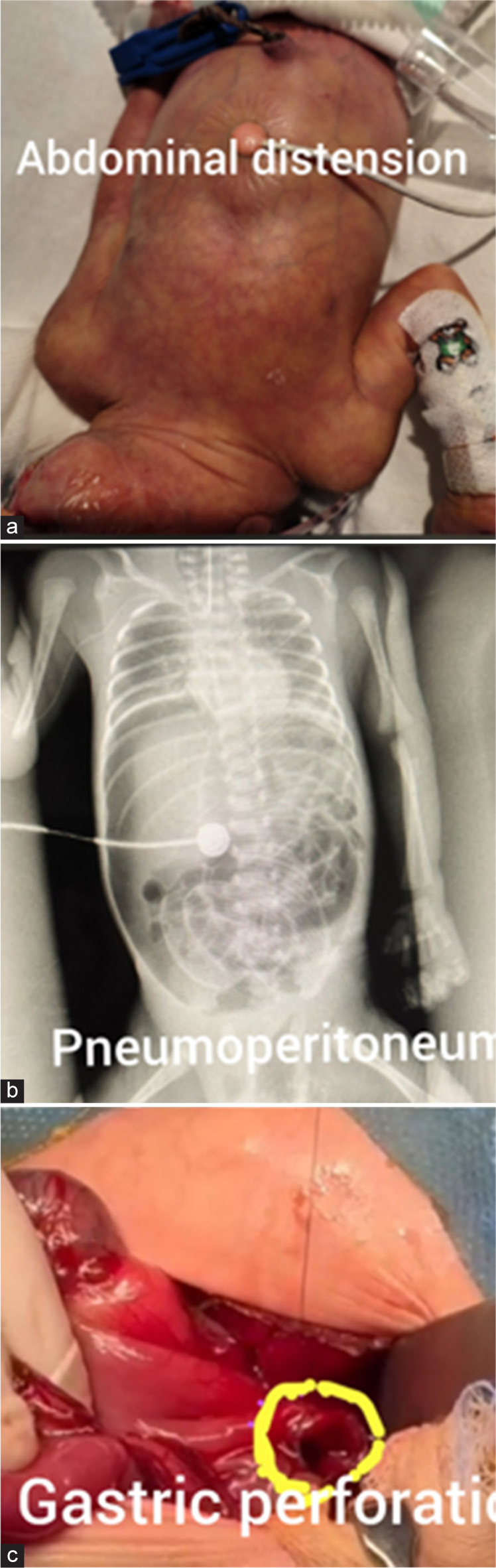
- (a) Preterm neonate with abdominal distension. (b) X-ray chest and abdomen showing air under the diaphragm. (c) Perforation in the stomach (yellow circle).
At around 50 h of age, he developed tachycardia with blood pressure maintained and he showed decreased left ventricular output on echocardiography, indicating compensated shock. His tummy was also distended. He was ventilated and kept nil orally sent blood for septic markers and started on Inotropes after fluid bolus. The C-reactive protein was high and within a few hours, the blood culture grew Klebsiella pneumoniae. He was started on ceftazidime-avibactam and aztreonam as the organism was carba-resistant. To confirm the type of resistance, a Carba R assay is done but in our case, we could not check. His abdominal X-ray showed gas under the diaphragm, indicating pneumoperitoneum [Figure 1b]. Immediately, the laparotomy exploration was performed and there was a perforation in the anterior wall near greater curvature extending to the fundus [Figure 1c]. The repair was done and shifted to the neonatal intensive care unit. After a few hours, he continued to be hypotensive with no urine output and severe metabolic acidosis not responding to the therapy, and succumbed to the illness.
DISCUSSION
Gastric perforation in neonates is not common and it has poor prognosis.[1] Many reasons including gut ischemia, the increased acid content of the gut, the absence of gastric musculature, necrotising enterocolitis, trauma and surgical conditions of the gut, including duodenal web and malrotation of the gut may cause gastric perforation with no single cause is considered.[2] The infection is the most common cause of gastric perforation. Capillary leak syndrome secondary to sepsis can also cause perforation.in our index case, he developed gastric perforation and also he was septic growing multi-drug resistant K. pneumoniae in the blood. The majority of the neonates are well at birth, feeding well and passing stools and suddenly become sick when perforation occurs as was seen in our case. He was taken to the operation theatre and an emergency laparotomy was performed in an attempt to save him but he succumbed postoperatively despite all the support. Retrospectively, this also made us think that bedside peritoneal drain would have been considered before taking to laparotomy. The evidence has shown that perforation can be managed conservatively with success. Leucopenia, hyponatremia metabolic acidosis, high lactate level, thrombocytopenia and male gender are risk factors associated with poor prognosis.[2] In a large cohort study, 40% of neonates died post-laparotomy procedure indicating a potential risk of surgery.[3] All these parameters were present in both the twins in our case but the male neonate developed perforation of the stomach and died. In our case, gender also must have made the difference, as it is known that males have a poor prognosis. Prematurity and low birth weight increase the mortality by 2 fold compared to term and appropriate gestational age.[4-7] The release of bacteria after the perforation can lead to bacterial peritonitis and the sepsis will cause a systemic inflammatory reaction hampering the tissue perfusion and leading to organ failure. The girl twin also became unwell growing the same organism K. pneumoniae in the blood on relevant antibiotics and getting better but never showed symptoms and signs of perforation.
CONCLUSION
Gastric perforation is an emergency needing surgical intervention including medical stabilisation. It also highlights the importance of selecting the case for either bedside peritoneal drain or exploratory laparotomy and repair depending on the stability of the neonate.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Neonatal gastric perforation: Case series and literature review. World J Surg. 2018;42:2668-73.
- [CrossRef] [PubMed] [Google Scholar]
- Gastric ischemia: The primary factor in neonatal perforation. Clin Pediatr (Phila). 1973;12:219-25.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for mortality in neonatal gastric perforation: A retrospective cohort study. Front Pediatr. 2021;9:652139.
- [CrossRef] [PubMed] [Google Scholar]
- Successful conservative treatment of intestinal perforation in VLBW and ELBW neonates: A single centre case series and review of the literature. BMC Pediatr. 2019;19:255.
- [CrossRef] [PubMed] [Google Scholar]
- The scare 2023 guideline: Updating consensus surgical Case report (SCARE) guidelines. Int J Surg. 2023;109:1136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal gastric perforation: Report of 15 cases and review of the literature. Pediatr Neonatol. 2008;49:65-70.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal sleeve gastrectomy for multiple gastric perforations: A case report. J Neonatal Surg. 2017;6:10.
- [CrossRef] [PubMed] [Google Scholar]






