Translate this page into:
Healthcare Innovation and Design Thinking
*Corresponding author: Gunda Srinivas Consultant-Pediatric Emergency & Pediatrics, Aster RV Hospital, JP Nagar, Bengaluru, Karnataka, India. srinivaspapadoc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Srinivas G. Healthcare Innovation and Design Thinking. Karnataka Paediatr J 2021;36(2):87-93.
Abstract
The objective of this article is to bring awareness to the changing landscape of the healthcare ecosystem and the clinician’s role with respect to medical devices, medical systems, technology, and processes involved in the system. Clinicians interact with them every day and have a huge implication for them directly, and to their patients indirectly. Clinicians are actively involved in clinical research which involves the knowledge and practice of the disease, diagnosis and management, etc. Recently, the role of non-clinical aspects such as medical devices, processes and systems of the healthcare ecosystem is gaining popularity. Hence, there is potential to explore this aspect of the healthcare delivery system to redesign and innovate for improving clinical outcomes. To achieve this, the clinicians need to understand these systems from a perspective that will help them to identify the problems and develop innovative solutions. Just like the clinical research is systematic and methodical, the improvement of the medical systems is also methodical to a large extent. This includes concepts and techniques that are quite fresh and new to a clinician who probably has never been exposed to these in their medical careers. These general principles of Innovation and Design thinking applied to other domains have yielded fantastic results and for the same to be applied in the medical domain, the role of the practicing clinician is central. As clinicians, we have always practiced innovation at some point of time in our career when we would have faced a resource crunch and were compelled to save the children and hence have tried to innovate on the devices, processes, etc., in our own way and has worked many a times. To generate many such solutions at large scale, the whole process needs to be methodical and systematic so that the solutions developed are safe and consistent at all times. Such a solution can be scaled up and made to reach across such setups where it is needed and there can be a measurable improvement in efficiency, quality, effectiveness, or economics of patient care delivery on a large scale.
Keywords
Healthcare innovation
Healthcare design thinking
Health system innovation
Medical innovations
WHAT IS CREATIVITY AND INNOVATION?
Creativity[1] is the ability to transcend traditional ways of thinking or acting, and to develop new, original ideas, methods, or objects. This ability comes from perception of the world in new ways, understanding hidden subtle patterns and make connections between seemingly unrelated things which lead to a new set of ideas and solutions.[2]
Innovation means to develop a new solution or introduction of new things/methods to solve any problem. It is the practical application of creativity that adds value to a product or service. Creativity is the basis of innovation.
Some other related terms to innovation are:
Invention[3] means creating something that has never been made before, or the process of creating something that has never been made before.
Jugaad is a very common Hindi word, meaning a cheap, improvised but effective solution to a problem inspite of limited resources born out of human ingenuity and cleverness. It can also be called a hack in terms of solving problems.
We need innovation in healthcare as well to solve old existing and new age problems, primarily to improve user (patient in healthcare domain) experience, clinical outcomes, and to make the care delivery more economical.
TYPES OF INNOVATION
Innovation[4] can be classified in various ways like, for example: We have various classifications of cerebral palsy by etiology, topography, etc.
Let’s highlight a few types to get a glimpse of how it can be extrapolated into the healthcare domain.
Based on the novelty of the solution and the impact it can create on the market, four types of innovation are described in Figure 1:
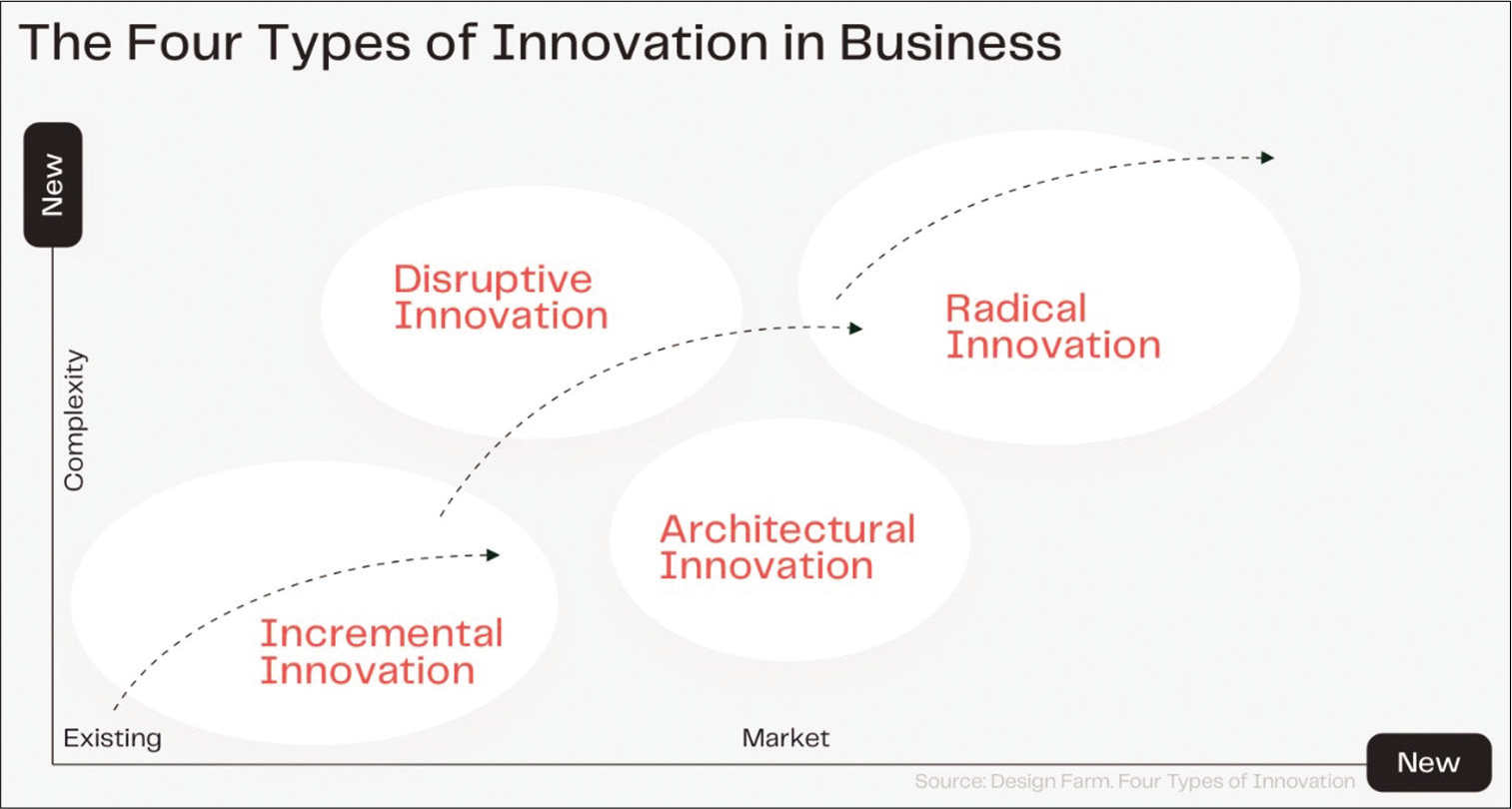
- Types of innovation.
Incremental Innovation
Constantly improving the existing products and services to add value.
It mainly focuses on reducing the shortcomings in design, adding new features, comfort, reducing costs or building next generation products.
This is short lived and of low impact, but helps the company to stay relevant.
Ex: Next series of BMW cars, new mechanical ventilators with better user interface and safety features. newer compact phototherapy devices, newer infant warmers with better efficiency.
Architectural Innovation
Modifying the existing products to suit to an entirely new user segment of market
It refers to changing the overall design of a product by putting existing components together in new ways
This innovation occurs in the short to medium term.
Ex: Sony Walkman, Desktop photocopiers, pre-operative practice using 3D models to shorten surgeries. high flow nasal cannula oxygen delivery systems in NICU, PICU.
Disruptive Innovation
First coined by well-known expert Clayton Christensen in one of his bestseller Innovator’s Dilemma, it is a very novel solution, concept, product, or a service that transform expensive, complex and sophisticated solutions into ones that are simpler, more convenient and affordable.
It happens when new technologies and products are created to serve an existing market.
This type of innovation is usually enabled by advent of new technology as an effective and economical alternative to what is already existing in the market. Disruptive innovation mostly originates at the lower end of the market segment; however, as the maturity of the technology increases, it eventually displaces established market leaders.
This innovation occurs in the medium to long term.
Ex: Peer-to-peer travel platforms-Airbnb, Digital photography, Point-of-care Ultrasound (POCUS) bringing compact bedside USG to intensivists and ER physicians, Telemedicine coupled with remote patient monitoring and smartphone-based devices as diagnostics.
Radical Innovation
When an organization applies new technology to a new market.
This type of innovation happens when a new product, process, or service with high technological advancement has a high market impact and eventually replaces an existing provider.
This innovation occurs in the long-term.
Ex: Electric vehicles, SpaceX developing reusable vehicles for space travel, 3D printing of bones in maxillofacial and orthopedic surgeries, Artificial Intelligence applied to healthcare data for disease epidemiology and prognostication, drones in healthcare, genome sequencing for disease management, etc.
Based on where exactly the innovation happens, innovations can also be classified as:
Product Innovation
There are improvements in performance characteristics and features of the products or devices.
Ex: Introduction of ultrasound technology, infrared vein finder, embrace warmer bags for newborn babies, etc.
Process Innovation
There is an implementation of a new or significantly improved research process, production, or delivery method.
Ex: The COVID vaccine innovation[5] developed by many companies was possible because of a change in the methodology/process of figuring out the right vaccine component like mRNA, mass producing it for millions in short time, The whole process to deliver the vaccine using the Co-WIN technology platform in India, healthcare simulation used to train medical and paramedical personnel.
Technology Innovation
This is where a new technology is being applied may be with a new product as well to solve problems in various domains.
Ex: The telemedicine system, virtual reality application in rehabilitation, application of 3D printing technology to printing bones, prosthesis, tissues, etc.,
Business model Innovation
Business model is nothing but a plan for the successful operation of a business, identifying sources of revenue, the intended customer base, products, and details of financing. This type of innovation is the easiest in terms of the resources required to implement it, but most complicated since it involves a deeper understanding of the customer (a patient in our case) to what exactly they need/want/would love to have but nobody understood them well till now. Here, a new business model is innovated with a fundamental change in how a company delivers value to its customers.
Ex: Pristyn care clinics which are chain of surgical clinics who rent the operation theaters (OTs) in less busy hospitals at nominal cost. They utilize this capacity and add their expertise in insurance, equipment, surgery and patient care practices, providing surgical services with same standard of care to patients without building any of hospitals or OTs. They intend to be better than corporate hospitals but 40% cheaper, Uber in transport, Swiggy in food delivery, and AirBnb in hospitality are all examples of newer disruptive business models.
CLINICIANS AND HEALTH SYSTEMS
Current health systems
Now that we understand what innovation means, let’s see how the healthcare domain operates. The clinicians and paramedical personnel are the main people involved in the care delivery with people of other domain expertise supporting the system. Clinicians are the important stakeholders who understand the ground reality and the pain points of the system. But the paradox is, clinicians are largely not involved in the designing or setting up of such systems. Clinicians have come to accept that the systems work in the way they work including the ingrained problems in them and continue to work with those problems or inefficiencies during the care delivery. They are unaware that, these are problems that can be solved with newer technologies and hence a status quo is maintained. To put it in a medical perspective, If you can’t identify a symptom or not aware of the diagnostic criteria, how can you diagnose a disease? This might not change unless either the clinician develops a new perspective to understand the system or the system is handled by others who can work closely with the clinicians and have the capability to solve them. Conventionally, clinicians’ primary responsibility has been patient care and anything else is not given much importance. Clinicians are very much involved in clinical research which includes the disease management, protocols, patient outcomes, and related aspects. However, what about the other parts of the care delivery such as the medical devices, existing processes, adoption of newer technologies, business models, and patient engagement which also impact patient care although indirectly? The clinicians are not formally trained in these aspects and hence not aware of how to handle these issues. They largely end up handing over these responsibilities to people of other domains who are not aware of the practical pain points and hence unable to improve them in an efficient way. These non-clinicians might develop some newer devices, implement newer systems, etc., which might not suit the clinical needs or might not be adopted well, usually ending up as failures.
The Innovative Clinician
Humans in general are innovative in nature but is not expressed unless pushed or they happen to work in adverse/ resource limited settings/scenarios. This applies to clinicians as well. For example: In the management of respiratory distress syndrome (RDS) in newborns, when the standard continuous positive airway pressure (CPAP) devices were not widely available, we have at many instances designed and assembled a simple bubble CPAP system using the urine collection bag and tubings connected to a T-piece and oxygen supply. This has worked reasonably well in the management of the RDS in term and preterm newborns and many would agree with it.[6,7] Another example is the use of styrofoam boxes as baby warmers especially for preterm/LBW babies in home setting, PHCs, during transport.[8]
Now, what if a clinician applies their innovative potential in solving other problems of the system? It is easier said than done because, in earlier scenarios, a clinician is able to solve clinical problems as he has in-depth knowledge. He knows what is needed to deliver that specific intervention either with an available device or could ingeniously assemble from commonly available resources of which he has prior knowledge of. Hence, he will not be able to innovate if his understanding of the problem is poor/ biased, prior knowledge of such resources is limited or his way of thinking is not suitable to identify the problem at all at first stage. This is the exact scenario of the clinician’s current inability to handle other aspects of the healthcare ecosystem. Examples like a simple appointment system, digital tools in the management of chronic diseases, many new medical devices playing a significant role in healthcare ecosystem, are being designed by the incumbent nonclinicians.
PATTERNED THINKING- SCHEMAS
Schemas
Humans naturally develop defined patterns of thinking modeled on daily, repetitive activities, and commonly accessed knowledge. These assist us in quickly applying the same actions and knowledge repeatedly in similar or familiar situations. These patterns of thinking are often referred to as schemas,[9] which are organized sets of information and relationships between things, actions, and thoughts that are stimulated and initiated in the human mind when we encounter some common environmental stimuli.
Advantages
We as clinicians also have schemas or so-called spinal reflexes which help us to identify common set of symptoms, disease patterns, clinical signs, and assist in implementing the disease management schemas fast without taking much time. In a way, the schemas help us to be efficient and save time and energy for more complex acts.
Limitations
Schemas also have the potential to stop us from accessing or developing new ways of seeing, perceiving, understanding, and solving problems. We need to understand when schemas do not work and need to develop a different way of perceiving things. As long as the patients respond well clinically and there is no other complex underlying condition missed by the initial diagnostic schemas, they work well. Our higher centers kick in when there is some deviation in clinical course and that is when we start to deeply analyze the clinical scenario again. These schemas or patterned thinking prevent us from diagnosing a complex condition or understanding a complex problem. In particular, experts and specialists rely on their solid thought patterns, and it can be very challenging and difficult for experts to start questioning their knowledge, or schemas.
To illustrate the limitations of schemas, take this for example: Some years ago, an incident occurred where a truck driver tried to pass the truck under a low bridge. But he failed, and the truck got stuck firmly under the bridge causing massive traffic jams, which resulted in emergency personnel, engineers, firelighters, and truck drivers gathering to devise and negotiate various solutions for dislodging the trapped vehicle. Emergency workers were debating whether to dismantle parts of the truck or chip away some part of the bridge. Each spoke of a solution which fitted within his or her respective level of expertise. A boy walking by and witnessing the intense debate looked at the truck, at the bridge, then looked at the road and said nonchalantly, “Why not just let the air out of the tyres?” to the absolute amazement of all the specialists and experts trying to solve the problem. When the solution was tested, the driver was able to drive away the truck with ease. The story symbolizes the struggles we face where oftentimes the most obvious solutions are hardest to come by because of the self-imposed constraints we work within. Time has come for clinicians to breakout of these schemas and think fresh.
DESIGN THINKING
Design thinking[9] is basically the way a designer would think while designing a product by being in the user’s position and empathizing with user on what exactly they would feel, need, and like. Some of the world’s leading brands such as Apple, Google, Samsung, and GE, have rapidly adopted the Design thinking approach, and is also being taught at leading universities around the world, including the Stanford, Harvard and MIT. “Design is not just what it looks like and feels like. Design is how it works.” quotes Steve Jobs, founder of Apple Inc.
Design thinking is a repetitive process in which we seek to understand the people (users of the end product/service), challenge our existing assumptions, and redefine problems in an attempt to identify alternative strategies and all possible solutions in an unbiased manner. These solutions might not be instantly apparent with our initial level of understanding/ schemas. It revolves around a deep interest in developing an understanding of the people for whom we are designing the products or services. It helps us to observe and develop empathy with the target user. It helps us in the process of questioning: questioning the problems, assumptions, and implications without bias.
Design thinking is extremely useful in tackling problems that are ill defined or unknown like that of healthcare, by
Understanding the user (patient in our case) and re-framing the problem in human-centric ways.
Creating many ideas in brainstorming (focused, repetitive, and iterative process) sessions.
Adopting a hands-on approach in prototyping (sketching, creating working models, and mock runs).
Testing and trying out the concepts and ideas.
All variants of Design thinking embody the same principles, which were first described by Nobel Prize laureate Herbert Simon in The Sciences of the Artificial in 1969. Let’s discuss the 5-phase model proposed by the Hasso-Plattner Institute of Design at Stanford, which is also known as d.school which is shown in Figure 2:[10]
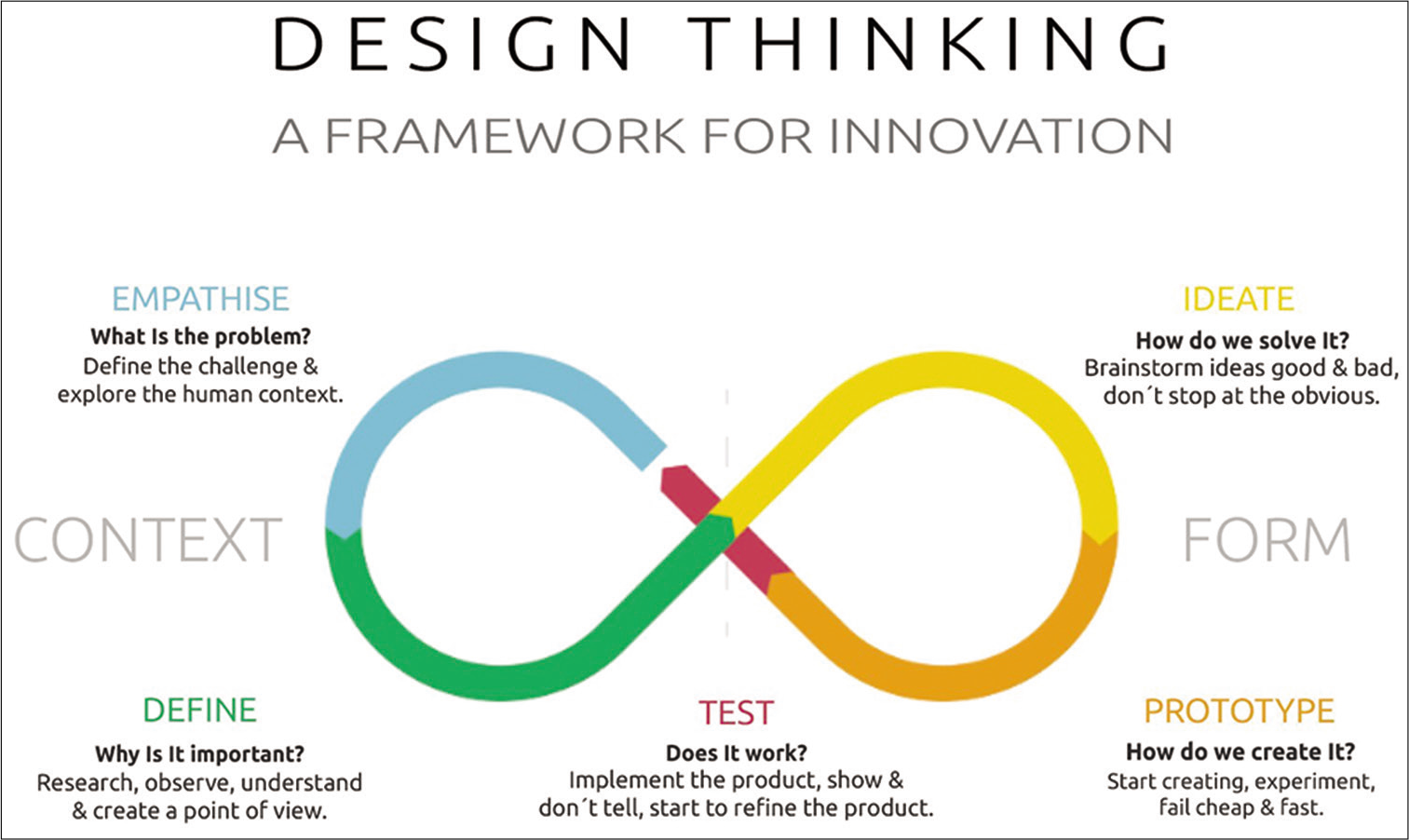
- 5 Steps of design thinking.
Design thinking is often referred to as “outside the box” thinking, as designers are attempting to develop new ways of thinking that do not abide by the dominant or more common problem-solving methods. It is not only to find the right solutions but also the ability to ask the right questions as well.
Empathize
To connect with the users and understand the problem from a user perspective in real sense which might include spending focused time with them, being the user themselves and observing to understand what exactly they go through and understand the problem inside out.
Define
To define your users’ needs, their problems, and your insights very clearly and in detail is very crucial. “Five Whys” approach (asking ‘Why?’ 5 times in a sequence) is used to get to the root cause which might be a good way to understand a problem, it is like the conventional history taking for any symptom to get to the probable diagnosis. Most important of all, is that the process is repetitive and expansive. Define clear problem statements as the outcome. Do not think of the solutions in this stage.
Ideate
Goal is to ideate by challenging assumptions and create ideas for innovative solutions, as many as possible in an unbiased manner. Designers resist the temptation to jump immediately to a solution to the stated problem. Brainstorming is the key to engage collaborative, multi-disciplinary teams to apply their perspectives, skills, personalities, and thinking styles of many to solve multifaceted problems. Only then will they finally converge upon their solutions. This is the essence of “Design Thinking.”
Prototype
Start creating some rough working models of product solutions using commonly available resources or doing a mock run of new process to understand how they might perform in real world.
Test
Very crucial is to test the solutions with the prototypes and get feedback and again repeat the process. This continues with assessing whether you could find answers to the questions you asked, ideate, and brainstorm solutions again.
DESIGN THINKING AND HEALTHCARE
Design thinking tries to empathize with human beings and involves ambiguous or inherently subjective concepts such as emotions, needs, motivations, and drivers of behaviours. This is very much true to the healthcare domain as well. The end users are the patients who are distressed and all they need is the support to get better. Healthcare domain has a lot to gain from design thinking. Well known physicians of the past have always preached us to see the patient and understand them as a whole that was probably design thinking applied to patients and all the clinical knowledge we have today is the result of that way of thinking.
Design thinking can be applied in two ways in healthcare
To solve the problems of the healthcare delivery system helping the clinician perform better using better devices, processes, and efficient systems.
To help patients as well, by designing products around them to make them part of the care delivery process such as chronic care apps, rehabilitation devices, and self-monitoring wearables etc.
The challenge today is that, design thinking needs to be applied by the clinician himself to the care delivery systems because, it would be impractical for the existing design thinkers to learn medicine, let them gain clinical experience and later apply it. Instead, the clinicians who face the problems can be taught design thinking approach. This article is all about sensitization to that need and develop such a newer approach which can enable us to see our systems with the design thinking glasses. It might happen that a design thinking clinician might start pointing out many critical problems in the system which can always be solved once identified. Some examples of applied design thinking in healthcare are:
Health-care simulations systems for better training and preparedness to reduce errors and improve preparedness and management.
Redesigning MRI console with theme of an adventure trip that excited kids rather than scare them and reducing the need to sedate or delay the scans at Pittsburg hospital.[11]
Designing the Pediatric Emergency Unit at Aster RV hospital, JP Nagar, Bangalore with the theme of a train (outside and inside) with a colorful ambience and distraction systems to reduce the fear, anxiety associated with visits to emergency rooms and make it a better experience to children and parents as well.
The number entry system on infusion pumps became more user centric with application of design thinking. A study found that 1000, 100, and 50 were most commonly used numbers but entry of these numbers was cumbersome in existing pumps until this study helped to understand the user, who is primarily the nurse at bedside.[12]
Peripheral intra venous (IV) line fixation using splints increased the life-span of the IV line.[13]
CONCLUSION AND THE WAY FORWARD
It is time to organize more events for the clinicians to get to understand design thinking in-depth, through workshops, active discussions, and hands-on experiences.
Multidisciplinary/cross domain interaction needs to be encouraged so that clinicians get exposed to various newer technologies, perspectives, and potential solutions that can be applied in the clinical domain.
Appropriate validation for safety standards and consistency is a must through suitable clinical trials before commercializing or propagating it.
Collaborate with technical domains, institutions, and work together to co-create solutions as a team.
Acknowledgements
I acknowledge my teachers, mentors, patients, and family who have given all these insights, learnings, and newer opportunities to further our learnings.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.99designs.com/blog/creative-thinking/what-is-creativity [Last accessed on 2021 Jun 11]
- What is Creativity? And Why is it a Crucial Factor for Business Success? 2021. Available from: https://www.creativityatwork.com/2014/02/17/what-is-creativity [Last accessed on 2021 Jun 23]
- [Google Scholar]
- Cambridge Dictionary. 2021. Available from: https://www.dictionary.cambridge.org/dictionary/english/invention [Last accessed on 2021 Jan 23]
- [Google Scholar]
- Available from: https://www.theworldwecreate.net/insights/four-types-of-innovation-in-business [Last accessed on 2021 Jun 11]
- Available from: https://www.nature.com/articles/d41586-020-03626-1 [Last accessed on 2021 Jun 12]
- Bubble continuous positive airway pressure machine versus indigenous bubble continuous positive airway pressure as a respiratory support in preterm babies with respiratory distress syndrome: A prospective outcome research at a tertiary care Centre in Gujarat, India. Int J Contemp Pediatr. 2018;5:493-8.
- [CrossRef] [Google Scholar]
- Efficacy of indigenous bubble CPAP in neonates with respiratory distress. Asian J Clin Pediatr Neonatol. 2019;7:6-8.
- [CrossRef] [Google Scholar]
- Reinforcing kangaroo mother care uptake in resource limited settings. Matern Health Neonatol Perinatol. 2018;4:26.
- [CrossRef] [PubMed] [Google Scholar]
- What is Design Thinking and Why Is It So Popular? 2021. Available from: https://www.interaction-design.org/literature/article/what-is-design-thinking-andwhy-is-it-so-popular [Last accessed on 2021 Jan 23]
- [Google Scholar]
- Available from: https://www.medium.com/intivedevelopers/the-5-stages-of-design-thinking-and-specific-techniques-da26f82e80bf [Last accessed on 2021 Jun 12]
- From Terrifying to Terrific: Man Redesigns MRI Machine to Delight Children Instead of Scare Them. 2021. Available from: https://www.goodnewsnetwork.org/terrifying-terrific-man-redesigns-medical-machine-delight-children-instead-scare [Last accessed on 2021 Jan 23]
- [Google Scholar]
- Designing devices with the task in mind: Which numbers are really used in hospitals? Hum Factors. 2013;55:61-74.
- [CrossRef] [PubMed] [Google Scholar]
- A randomised controlled trial on effect of splinting a joint on the lifespan of intravenous cannula in pediatric patients. Int J Contemp Pediatr. 2020;7:1092-5.
- [CrossRef] [Google Scholar]






