Translate this page into:
Latex allergy in healthcare workers: A review
*Corresponding author: Kavita Yadav, Department of Paediatrics, Sir Gangaram Hospital, Delhi, India. drkavita1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav K, Gupta N. Latex allergy in healthcare workers: A review. Karnataka Paediatr J 2023;38:110-6. doi: 10.25259/KPJ_44_2023
Abstract
Allergy to latex is one of the reported concerns among healthcare workers. It has been found in various studies that latex sensitivity is 3–5 times higher in doctors and nurses as compared to non-healthcare workers. The main source of latex allergy is exposure to powdered gloves. Chronic exposure to latex can lead to various symptoms such as pruritus, dermatitis, erythema and urticaria, rhinitis, conjunctivitis, and asthma. There is sparse Indian data due to a lack of awareness and diagnostic facilities; therefore, studies are required to evaluate latex-related symptoms and sensitisation with the use of powdered gloves as compared to the use of non-powdered gloves and to institute appropriate preventive strategies.
Keywords
Latex allergy
Healthcare workers
Latex
INTRODUCTION
Allergy to latex is one of the reported concerns among healthcare workers. It has been found in various studies that latex sensitivity is 3–5 times higher in doctors and nurses as compared to non-healthcare workers. The main source of latex allergy is exposure to powdered gloves. Chronic exposure to latex can lead to various symptoms such as pruritus, dermatitis, erythema and urticaria, rhinitis, conjunctivitis, and asthma. There is sparse Indian data due to a lack of awareness and diagnostic facilities; therefore, studies are required to evaluate symptoms associated with latex and sensitisation with the use of powdered gloves as compared to that of non-powdered gloves and to institute appropriate preventive strategies.
BACKGROUND
The history of latex goes back to 1650 BC when it was first used in indigenous cultures of Mesoamerica, where it was used to make balls for Mesoamerican ballgames. Later, latex sap was used for making waterproof textiles and containers in Maya and Aztec cultures.[1] In 1736, Charles Marie introduced rubber samples in France and published the first scientific paper on rubber properties in 1755.[2] In 1770, Joseph Priestley coined the term ‘rubber’ and discovered that it was extremely useful in rubbing off pencil marks on paper. Francois Fresnau, in 1764, discovered that turpentine was a rubber. In 1779, Giovanni Fabbroni discovered that naphtha was a rubber solvent. In 1839, Charles Goodyear redeveloped vulcanisation.[3] Charles Macintosh, in 1823, made waterproof garments by dissolving rubber in coal-tar-naphtha and called them Macintosh Garments, also known as the first raincoats. South America remained the main source of latex rubber used during the 19th century. Henry Wickham, in 1876, smuggled 70,000 Amazonian rubber tree seeds from Brazil and delivered those seeds to England. These seeds were further sent to India, Malaya, and other countries.[4] In the last two centuries, the world has seen globalisation and industrialisation in the field of the rubber industry. In India, commercial cultivation of rubber was started by British planters, and the first commercial Hevea plantation was established at Thattekadu in 1902 in Kerala. India, today, is the world’s third-largest producer and fourth-largest consumer of rubber.[5]
LATEX
Latex is a suspension and is commercially obtained from the milky sap of the Hevea brasiliensis plant, which is known as the rubber tree.[6] The rubber tree is grown largely in Africa and Central Asia.[7] The manufacturing, curing agents (such as ammonia), accelerators (e.g., thiurams and carbamates), antioxidants, and stabilisers are added to liquid latex so as to give the product its final shape, colour, shape, and texture.[8]
Natural rubber latex (NRL) contains more than 240 protein peptides. Fifteen allergens – Hev b1 to Hev b15, are identified and well well-characterized.[9] The major allergens which are found in healthcare workers with latex allergy are Hev b5 and Hev b6. Protein allergens in latex include patin and havamine. Throughout the manufacturing process, these proteins remain on the surface of the latex product and are released during the use of the product, which leads to latex allergy.[10]
The global production of latex has increased significantly over the years as latex is being used widely in everyday basic needs. The manufacturing of some latex products, such as gloves, condoms, and balloons, involves a process of dipping, which consequently exposes the users to very high quantities of latex protein.[11]
The dipping method involves the use of glove-shaped moles, which are dipped in liquid latex to make the glove. The dipped products expose users to a higher quantity of latex due to the large surface area to volume ratio of gloves; hence, it increases the risk of sensitisation/reaction.
Corn starch (a form of powder) is usually used in latex gloves, which restricts the surfaces from sticking to each other. Therefore, this makes it easier for users to wear latex gloves. In powdered gloves, the latex is absorbed readily into powder. The use of powder/corn starch in latex gloves has the chances of exposure through inhalation.[12]
Latex has been used for making gloves due to its excellent characteristics, such as tactile qualities, comfort, barrier production, and sterility. Other qualities include resealing ability and flexibility.[13]
Other than gloves, latex has been used widely in healthcare. Products containing latex includes urinary and intravenous catheters, tape adhesive, intravenous tubing ports, syringe plungers, intravenous bags and medication vial needle ports and masks, to name a few. In home, products which contain latex include disposable diapers, toys, condoms, diaphragms, balloons and carpet padding. It is also found in pacifiers, bottle nipples, sneakers, automobile tires, raincoats and boots.[14]
LATEX ALLERGY
Latex sensitivity is reported in <1% of non-atopic general population but reaches up to 5–15% among healthcare professionals.[15] This difference in prevalence is due to different diagnostic procedures or it may be associated with the frequency of use and quality of gloves.[16] Exposure to latex products occurs through contact with mucosal surface, skin and through respiratory tract.[17] The powdered latex gloves spread latex antigens in the working environment; hence, the allergen is powder.[18] Sensitised individuals may have systemic reactions or asthmatic reactions to airborne NRL proteins, which are associated with the use of powder.[19]
Latex allergy is a frequent occupational disease among healthcare providers and is the leading source of occupational allergies.[20]
NRL reactions can present in three forms: The first form is contact dermatitis on hands after wearing gloves, which is due to mechanical friction and drying. The second form is Type 1 immediate hypersensitivity reaction to latex, which is an immunoglobulin E (IgE)-mediated hypersensitivity reaction to latex. In this, the immune system makes IgE antibodies on exposure to latex allergen.[21] The immune system then prepares to react immediately to latex the next time the body comes in contact with latex. Now, when the sensitised person is re-exposed to the latex allergen, they develop allergic symptoms such as reddening of skin/ wheals, blistering, or/and wheezing. Type 1 reaction is the least common but is most life-threatening.[22] Immediate hypersensitivity is characterised by angioedema, scleral oedema, bronchospasm, lacrimation, angina, rapid heartbeat, and various other symptoms.[7] Moreover, the third form is allergic contact dermatitis, which is a type 4 delayed hypersensitivity reaction that involves the activation of T lymphocytes and results in tissue damage.[22] Type 4 reaction is characterised by contact dermatitis, erythema, vesicular lesions, contact urticaria, and eczema. The delayed allergic response to latex is mainly dermal.[23]
The routes of exposure are cutaneous, mucosal, parenteral, and inhalation.[24] Direct mucosal (i.e., mouth, nose, genitals, bladder, and rectum) and parental routes carry the highest risk of anaphylaxis.[25]
Powdered gloves increase the airborne protein inhalation in healthcare workers.[26] The powder in most latex gloves is made up of corn starch. The corn starch in powdered gloves is inhaled by the healthcare providers, and hence, the latex allergen is transported to the respiratory tract, which further leads to symptoms.[10]
SYMPTOMS WITH LATEX ALLERGY
The symptoms of latex allergy vary from contact dermatitis to severe anaphylaxis.[27]
The signs and symptoms of IgE-mediated reaction include contact dermatitis, rhinitis, asthma, and anaphylaxis reactions such as hypotension, circulatory collapse, and death.[28]
General signs and symptoms of an allergic reaction include itching and oedema around eyes, urticaria, rhinitis, nasal itching, wheezing, dermatitis and shortness of breath.[29] In individuals with latex sensitisation, immediate allergy or anaphylaxis may develop when these individuals are re-exposed to latex through the use of gloves, surgery, or some invasive procedure.[30] Delbourg et al.[31] and Bykowsky[12] reported signs related to latex allergy to be asthma, contact dermatitis, contact urticaria, rhino conjunctivitis, pruritus, oedema, conjunctivitis, eczema, erythema, and anaphylaxis. Brugnami et al.[32] also reported angioedema and laryngeal oedema.
AT RISK FOR LATEX ALLERGY
After the mandatory implementation of universal precautions in 1988, there has been an increase in reported allergy cases to latex.[33] The increase in daily glove use, along with frequent changing of gloves, has resulted in an increase in inhalation and contact with latex. These factors have resulted in an increase in sensitisation and, hence, an increase in occupationally acquired latex allergy.[6] One study reported that 62.5% of latex allergy-positive individuals had a previous history of atopy.[34] Atopy is an allergic predisposition that increases the risk of developing latex allergy in sensitised healthcare workers by 24%.[30]
Risk factors for developing latex allergy include:
Individual with multiple surgical procedures (patients with spina bifida)[7]
Healthcare providers, cleaners, and housekeepers
Electrician and motor mechanics
Workers in glove manufacturing plants[32]
Patients requiring frequent catheterisation[11]
Specific food allergies such as banana, avocado, chestnut, kiwi, and papaya have a higher degree of association with latex allergy due to cross-reaction.
According to Heinzerling and Johnson [11], the female gender is at higher risk of developing latex allergy. Another study has also reported that the risk of latex allergy is higher in children who play with rubber toys and glove-wearing dietary workers.[24]
It has also been reported that frequent hand washing by healthcare workers increases skin irritation, which further increases the risk for sensitisation to latex. In addition, warm/ wet skin tends to absorb latex proteins better than dry skin.[25] The presence of dermatitis facilitates the absorption of water-soluble antigens in latex, which leads to sensitization. Continuous exposure to latex in sensitised individuals may lead to a generalised IgE response.[35]
DIAGNOSIS AND INVESTIGATIONS
Diagnosis of latex allergy includes detailed medical history, physical examination, and supplemental testing as explained in Flow diagram 1.
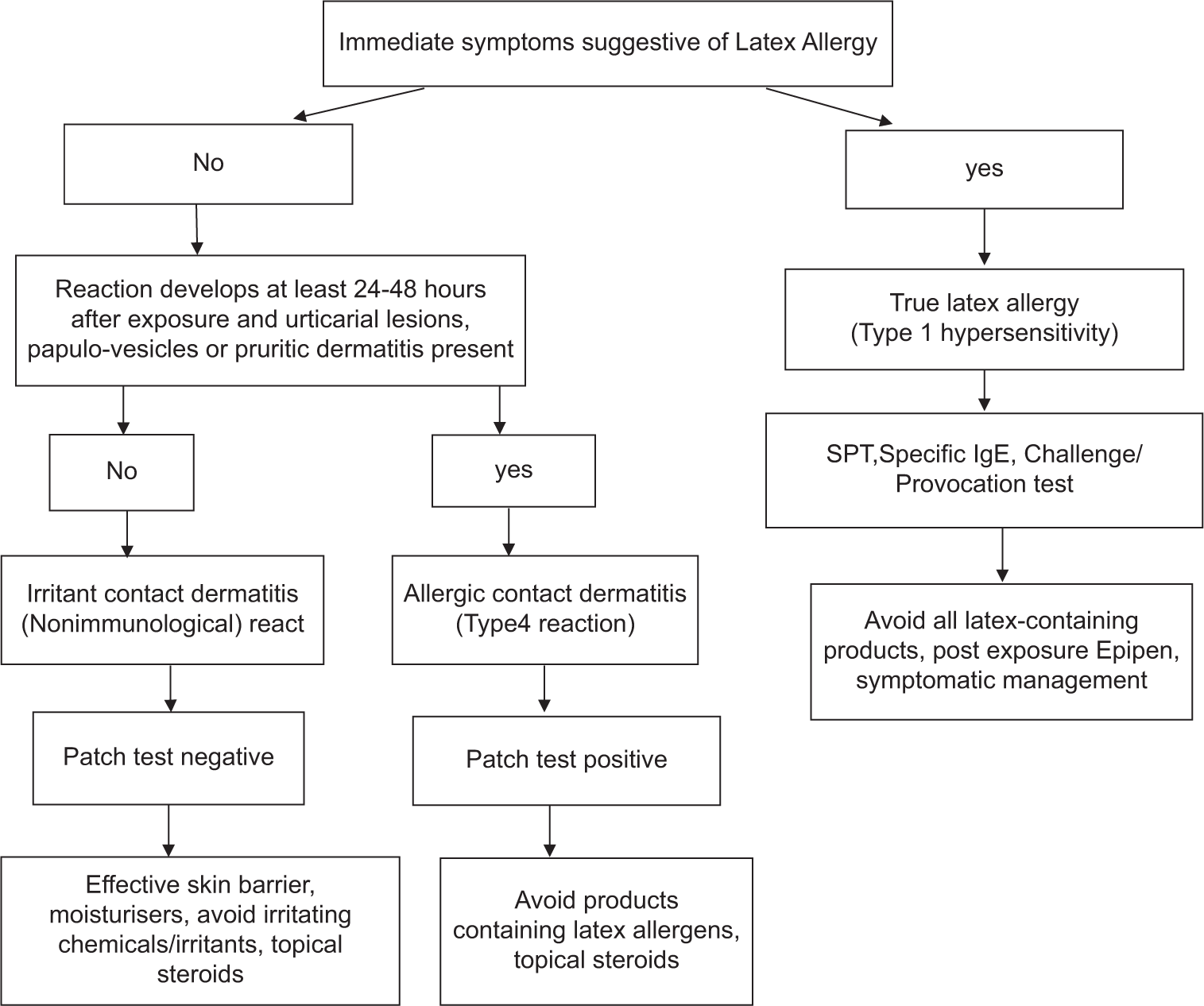
- Flow diagram for investigations and management in latex allergy.
Skin prick testing (SPT): The extract for the skin prick test is made by cutting the glove finger into small bits (approx. weight to 1 g). Dissolve this in 9 mL of saline for 15 min. Filter this solution with a normal filter paper. Now, use histamine and saline as controls. SPT is a safe and effective diagnostic technique when extracts are standardised for allergens and stability.[36]
Serology testing: Latex-specific IgE antibody serology with ImmunoCAP or Immulite system is a choice for diagnostic testing for food and drug administration. If the skin prick test/puncture is inconsistent with clinical history, then latex-specific IgE antibody serology assay can be followed by a skin prick test.[37]
Provocation test: It is usually discouraged due to the risk of anaphylaxis. It is performed when there is inconsistency with the patient’s history, latex-specific IgE antibody serologic test, and SPT results. The test should be performed with caution.[38]
Patch test: This test is used to differentiate dermatitis caused by IgE-mediated hypersensitivity reactions from cell-mediated hypersensitivity reactions to latex components in Hev b and chemicals added to rubber.[39] Positive patch testing is considered definite if patch testing with both products, the allergen, and the allergen are positive. The reaction is considered probable if the product used by the patient contains the positive allergen; ‘possible’ if the distribution of dermatitis matches the use of the product that typically contains positive allergen.
PREVENTION
Prevention can be – primary prevention or secondary prevention.
Primary prevention
The best way of preventing sensitisation and latex allergy is by avoiding the use of latex.[40] However, avoidance of latex is practically not possible in the current healthcare system. However, there are several ways to minimise exposure to allergens. Therefore, it is wise to select products that have low allergen content. The manufacturers are required to decrease the protein allergens in latex products to prevent the sensitisation of at-risk workers.[40] Whenever possible, atopic individuals should wear a non-latex liner inside latex gloves or a cotton liner. It is very important for individuals who wear latex gloves not to touch others who do not need to be touched.[41] In addition, they should eliminate the unnecessary use of gloves and wear them only when necessary so as to prevent exposure to body fluids or harmful chemicals. Latex gloves should not be stored in places where latex sensitive or allergic individuals are working.[13] Furthermore, only low NRL allergen gloves should be used by coworkers of healthcare workers with latex allergy. When powdered gloves are removed, the powder is aerosolised; therefore, powder free latex gloves should be used so that there is a decrease in airborne latex allergens.
It is also important to educate the individuals who use latex products, especially powdered latex gloves, to wash their hands properly and promptly after using the products. Effective hand washing is very important for preventing the spread of latex glove powder to other people and surfaces. Furthermore, the family members can be affected through contact with healthcare workers, who return home with latex powder on their surfaces and hands.[8]
Latex-free gloves are available in vinyl, plastic, and silicone. However, latex-free gloves do not provide good barrier protection from viral particles. Furthermore, non-latex gloves are more expensive as compared to latex gloves without providing the same degree of protection or tactile sensitivity. Reddy,[42] in their study, listed several latex-free gloves along with a comparison of cost to latex gloves. Table 1 describes the properties and comparison of various gloves.
| Latex | Nitrile | Neoprene | Vinyl | |
|---|---|---|---|---|
| Resistance | 5 | 5 | 5 | 1 |
| Biological protection | 5 | 5 | 5 | 2 |
| Chemical protection | 4 | 5 | 5 | 1 |
| Elasticity | 5 | 3 | 4 | 1 |
| Comfort | 5 | 2 | 4 | 3 |
| Sensitivity | 5 | 2 | 4 | 3 |
| Price | 3 | 2 | 1 | 5 |
5: Maximum score (in price, the cheapest), 1: Minimum score (in price, the most expensive)
Secondary prevention
At present, no immunotherapeutic regimens are available to prevent the development of latex allergy. Purified latex allergen can be useful for immunotherapy.[24] Till the time immunotherapeutic drugs are available for desensitisation, all atopic patients who are regularly exposed to latex should undergo latex allergy screening.[40]
Furthermore, latex items should be replaced by non-latex items, such as adhesive bandages with sterile dressing tapes with plastic tape, balloons with mylar balloons, blood pressure cuff tubing with rolled cotton batting on areas of contact with patients’ skin and other items as listed in the Table 2.
| Latex item | Non-latex form |
|---|---|
| Adhesive bandages | Sterile dressing with plastic tape |
| Adhesive tape | Plastic tape, paper tape, 1-inch rolled cotton gauze. |
| Adhesives | Non-latex adhesives |
| Anaesthetic circuits | Neoprene circuits, bags |
| Bite blocks | Silastic bite blocks |
| Balloons | Mylar balloons |
| Blood pressure cuff tubings | Rolled cotton batting on areas of contact with patients’ skin |
| Foleys catheter | Silastic Foleys catheter |
| Catheter leg bag straps | Velcro fastening tape straps. |
| Crutch auxiliaries and hand pads | Cover with cloth |
| Disposable diapers, rubber pants | Cloth diapers |
| Drains, penrose | Silicone tubings |
| Electrode pads | Non-latex brands |
| Esmarch bandages | White cotton ace bandages |
| Finger cots | Non-latex glove fingers |
| Gloves, Examination | Vinyl or nitrile gloves |
| Gloves, surgical | Neoprene, nitrile gloves. |
| IV tubing, rubber stoppers | Three-way stopcocks on IV tubing |
| Masks, moulded with elastic band | Other types of surgical masks |
| Medication vials with rubber stoppers | Use ampules if possible |
| Name bands | Non-latex name bands |
| Needle counting systems | Remove foam stick pad and use the magnetic side. |
| Pacifiers | Plastic or silicone pacifier |
| Rubber bands | String |
| Stethoscope tubing | Place cloth around the latex |
| Syringes | Glass syringe; latex-free syringe |
| Sheets | Disposable underpads |
| Solution bag injection port | Tape injection ports |
| Tourniquets | Wrap with stockinette or wrap over clothing |
| Toys | Cloth or vinyl toys |
| Wheelchair cushion | Cover with cloth |
CONCLUSION
Latex allergy is a cause of concern in healthcare workers, and public awareness is necessary to encourage individuals who are symptomatic to seek medical consultation for their problems. It is also very important to educate the families of allergic individuals about latex allergy and provide them with a list of common products and their latex substitutes.
Certain precautions in operation theatre should be taken, such as surgeries of individuals with known latex allergy should be scheduled as the first surgery case of the day. There should be the availability of latex-free carts for the care of latex-allergic clients.
The policies of healthcare workers must outline the steps in healthcare facilities that will educate and inform employees about products containing latex. Furthermore, it is important to outline the steps for handling employees with latex allergies or workers who may develop latex allergies during employment.
Ethical approval
The research/study complied with the Helsinki declaration of 1964.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Encyclopedia of American Indian contributions to the world: 15,000 years of inventions and innovations New York: Infobase Publishing; 2009.
- [Google Scholar]
- Charles Marie de la condamine. Available from: https://bouncing-balls.com [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Prehistoric polymers: Rubber processing in ancient Mesoamerica. Science. 1999;284:1988-91.
- [CrossRef] [PubMed] [Google Scholar]
- Natural rubber in India. 2016. Available from: https://web.archive.org/web/20161001100758/http:/www.dsir.gov.in/reports/ExpTechTNKL/Abs%20new/Rubber.htm [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Allergic reactions to latex among health-care workers. Mayo Clin Proc. 1992;67:1075-9.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of latex allergy and its implications for emergency nurses. J Emerg Nurs. 1996;22:29-36.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy precautions. A research-based protocol. Nurs Clin North Am. 1995;30:475-93.
- [CrossRef] [PubMed] [Google Scholar]
- Identification, cloning, and sequence of a major allergen (Hev b 5) from natural rubber latex (Hevea brasiliensis) J Biol Chem. 1996;271:25394-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cornstarch powder on latex products is an allergen carrier. J Allergy Clin Immunol. 1994;93:751-8.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy: One emergency department's response. J Emerg Nurs. 1996;22:67-9.
- [CrossRef] [PubMed] [Google Scholar]
- Barrier protection and latex allergy associated with surgical gloves. AORN J. 1995;61:1037-44.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy. A guideline for perioperative nurses. AORN J. 1992;56:488-93, 496-502
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of latex allergy in operating room nurses. J Allergy Clin Immunol. 1992;90:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy in primary care providers. J Investig Allergol Clin Immunol. 2011;21:459-65.
- [Google Scholar]
- Anaphylactic shock after game of squash in atopic woman with latex allergy. Lancet. 1990;335:1095.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergen sensitization and risk factors due to glove use by health care workers at public health units in Florianopolis, Brazil. J Investig Allergol Clin Immunol. 2007;17:27-33.
- [Google Scholar]
- Natural rubber latex allergy: A problem of interdisciplinary concern in medicine. Arch Intern Med. 2001;161:1057-64.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy: A follow up study of 1040 healthcare workers. Occup Environ Med. 2006;63:121-5.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational exposure of Brazilian neonatal intensive care workers to latex antigens. Allergy. 2004;59:107-10.
- [CrossRef] [PubMed] [Google Scholar]
- Shared 19B binding sites among separated components of natural rubber latex. Int Arch Allergy Immunol. 1996;111:48-54.
- [CrossRef] [PubMed] [Google Scholar]
- Allergens spur hospitals to offer latex-free care. Mater Manag Health Care. 1994;3:3-28, 30-2, 34
- [Google Scholar]
- Latex allergy review of 44 cases including outcome and frequency association with allergic hand eczema. Arch Dermatol. 1996;132:265-71.
- [CrossRef] [Google Scholar]
- Latex allergens in tire dust and airborne particles. Environ Health Perspect. 1996;104:1180-6.
- [CrossRef] [PubMed] [Google Scholar]
- Latex sensitivity. Controlling health care workers', patients' risks. AORN J. 1994;59:615-7, 620-1
- [CrossRef] [PubMed] [Google Scholar]
- Immediate allergy to rubber gloves: A questionnaire study of hospital personnel. J Dermatol. 1995;22:19-23.
- [CrossRef] [PubMed] [Google Scholar]
- Hypersensitivity to banana in latex allergic patients: Identification of two major banana allergens of 33 and 37 kD. Ann Allergy Asthma Immunol. 1996;76:321-6.
- [CrossRef] [PubMed] [Google Scholar]
- Work-related late asthmatic response induced by latex allergy. J Allergy Clin Immunol. 1995;96:457-64.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical glove powders bind latex antigens. Arch Surg. 1992;127:1354-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of latex-specific IgE antibodies in patients being evaluated for allergy. Ann Allergy Asthma Immunol. 1995;74:184-7.
- [Google Scholar]
- Latex allergy: A new threat to patients and health professionals. J Formos Med Assoc. 1996;95:361-3.
- [Google Scholar]
- In vivo sensitization to purified Hevea brasiliensis proteins in health care workers sensitized to natural rubber latex. J Allergy Clin Immunol. 2003;111:610-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic performance of Food and Drug Administration-cleared serologic assays for natural rubber latex-specific IgE antibody. J Allergy Clin Immunol. 1999;103:925-30.
- [CrossRef] [PubMed] [Google Scholar]
- Latex-specific proteins causing immediate-type cutaneous, nasal, bronchial, and systemic reactions. J Allergy Clin Immunol. 1992;89:759-68.
- [CrossRef] [PubMed] [Google Scholar]
- An 8-year retrospective review of patch testing with rubber allergens: The Mayo Clinic experience. Dermatitis. 2010;21:33-40.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy: Its importance in clinical practice. Allergy Proc. 1992;13:67-9.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy: Everyone is at risk. Plast Surg Nurs. 1995;1:204-6.
- [CrossRef] [PubMed] [Google Scholar]
- Latex allergy. 1998. American Family Physician. Available from: https://www.aafp.org/afp/98010Iap/reddy.htm [Last accessed on 2023 Jul 03]
- [Google Scholar]






