Translate this page into:
Occurrence of diabetic retinopathy in children with type 1 diabetes mellitus
*Corresponding author: Mohd Faisal Zoheb, Department of Paediatrics, Mahadevappa Rampure Medical College, Kalaburagi, Karnataka, India. faisalzoheb007@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Zoheb MF, Patil S, Angadi K, Mangshetty R. Occurrence of diabetic retinopathy in children with type 1 diabetes mellitus. Karnataka Paediatr J. 2024;39:150-4. doi: 10.25259/KPJ_44_2024
Abstract
Objectives:
Type 1 diabetes mellitus (T1DM) represents approximately 5–10% of all diabetes cases. Over time, nearly all individuals with T1DM are likely to experience diabetic retinopathy (DR). Within this group, the incidence of retinopathy is around 25% after 5 years of diagnosis, increasing to 60% after 10 years and reaching approximately 80% after 15 years. (1) To study the occurrence of DR in T1DM affected children and adolescents. (2) To study the relation of occurrence of DR with glycaemic control. (3) To study the relation between the duration of Type-1 diabetes and the occurrence of DR.
Material and Methods:
Following approval from the institutional ethics committee and informed consent from the parents of participating subjects, a prospective observational study was conducted involving 54 paediatric patients with T1DM from the outpatient and inpatient departments. A comprehensive history was documented for each participant, and screening for DR was performed using direct ophthalmoscopy. Glycaemic control was assessed by measuring glycated haemoglobin (HbA1c) levels, with findings recorded in a structured pro forma. Data were entered into Microsoft Excel and were analysed using IBM Statistical Package for the Social Sciences Version 25.0, with both qualitative and quantitative analyses conducted. A P < 0.05 was considered statistically significant.
Results:
The study analysed 54 children with type 1 diabetes, equally divided by gender, with a mean age of 12.72 years. The onset age was most common between 6–10 and 11–15 years, averaging 8.87 years. Most children (79.6%) had diabetes for 1–5 years, with a mean duration of 3.85 years. HbA1c levels were ≥8.5% in 83.3% of the children, averaging 10.6%. No children exhibited symptoms of DR, though 3.7% had DR. Significant associations were found between higher HbA1c levels, longer diabetes duration and the presence of DR (P < 0.05).
Conclusion:
The present study demonstrates a relatively low incidence of DR among children with diabetes. It underscores the significance of diabetes duration and HbA1c levels as contributing factors in Indian paediatric patients. Optimal glycaemic control is highlighted as crucial in mitigating the onset and progression of DR in young diabetics.
Keywords
Diabetic retinopathy
Glycated haemoglobin (HbA1C)
Diabetes mellitus
Type 1
Ophthalmoscopy
Paediatric patients
INTRODUCTION
Diabetes is a chronic, complex condition necessitating regular medical management with multifaceted strategies for risk reduction beyond glycaemic control. According to the World Health Organization, global diabetes prevalence has escalated from 108 million to 422 million in 1980–2014.[1]
Type 1 diabetes mellitus (T1DM) accounts for approximately 5–10% of all diabetes cases, resulting from the autoimmune destruction of pancreatic beta cells, with around three-quarters of diagnoses occurring in individuals under the age of 18.[2]
It is estimated that nearly 5 lakh children under 15 years old worldwide have type 1 diabetes, with significant regional variations in incidence.[3]
Diabetic retinopathy (DR), a microvascular complication associated with diabetes mellitus (DM), results from damage to the retinal capillaries and venules, making it the most prevalent microvascular condition amongst children with type 1 diabetes.[4]
Nearly all individuals with type 1 diabetes will eventually develop DR, with approximately 25% affected within 5 years of diagnosis, 60% within 10 years, and 80% within 15 years. After 15 years, around 18% of patients may progress to proliferative DR.[5]
The global incidence of diabetes has steadily risen over recent decades across all age groups, including youth, and this trend is projected to continue.[6]
This study aims to highlight the significance of DR occurrence in individuals with T1DM, which will, in turn, support the development of effective screening and management strategies for these conditions.
MATERIAL AND METHODS
Source of data
Data were gathered from confirmed cases of T1DM in patients under 18 years of age who attended the Outpatient Departments (OPDs)/Inpatient Departments of Basaveshwar Hospital and Sangameshwar Hospital, both affiliated with M.R Medical College in Kalaburagi, Karnataka.
Methods of data collection
Study design
Cross-sectional study.
Study setting
Department of Pediatrics - Basaveshwar Hospital and Sangameshwar Hospital, both affiliated with M. R Medical College in Kalaburagi, Karnataka.
Study cases
50 cases.
Sampling method
Simple random sampling.
Study duration
August 01st, 2022 –January 31st, 2024 (18 months).
Eligibility criteria
Patients under 18 years of age with confirmed T1DM, diagnosed according to the American Diabetes Association guidelines.[1]
Exclusion criteria
Other ophthalmological conditions such as hypertensive retinopathy and retinopathy of prematurity.
Methodology
Upon receiving clearance from the Institutional Ethics Committee and informed consent from patients, parents, or guardians, 54 subjects diagnosed with T1DM were enrolled in the study according to specified inclusion criteria.
A comprehensive history was obtained from each participant, covering details such as age at enrollment, age at initial Type 1 diabetes diagnosis, gender, duration since diagnosis, type of insulin used, and signs and symptoms of DR.
All patients are screened for DR by direct ophthalmoscopy in ophthalmology OPD.
Glycated haemoglobin (HbA1c) levels were measured from venous samples using high-performance liquid chromatography.
Data analysis
Statistical analysis was performed using IBM Statistical Package for the Social Sciences software version 25.0. Data collected were organised in an Excel spreadsheet to create a master chart, from which tables and graphs were generated. For quantitative data, mean and standard deviations were calculated, with the t-test applied to determine statistical significance. For qualitative data, the Chi-square test and Fisher’s exact test were used to assess significance. A P < 0.05 was taken as statistically significant.
RESULTS
The study investigated 54 children with T1DM to evaluate several aspects, including age, gender, duration of diabetes, glycaemic control and the prevalence of DR [Table 1].
| Variable | Category | Number of children | Percentage | Mean±SD | P-value and significance |
|---|---|---|---|---|---|
| Age distribution | 1–5 years | 4 | 7.4 | ||
| 6–10 years | 8 | 14.8 | |||
| 11–15 years | 28 | 51.9 | 12.72±4.04 | P=0.532, NS | |
| 16–18 years | 14 | 25.9 | |||
| Gender distribution | Male | 27 | 50.0 | ||
| Female | 27 | 50.0 | |||
| Age of onset of diabetes | 1–5 years | 11 | 20.4 | 8.87±3.82 | |
| 6–10 years | 21 | 38.9 | |||
| 11–15 years | 21 | 38.9 | |||
| 16–18 years | 1 | 1.8 | |||
| Duration of diabetes | 1–5 years | 43 | 79.6 | 3.85±2.49 | |
| 6–10 years | 10 | 18.6 | |||
| 11–15 years | 1 | 1.8 | |||
| HbA1c levels | <8.5% | 9 | 16.7 | 10.6%±2.37 | |
| ≥8.5% | 45 | 83.3 |
SD: Standard deviation, HbA1c: Glycated haemoglobin, NS: Non-significant
A majority of the participants (51.9%) were within the 11–15-year age range, while 25.9% were aged 16–18 years. The average age of the sample was 12.72 years, with no statistically significant difference observed between females and males (P = 0.532). The cohort comprised an equal distribution of females and males, each representing 50.0% of the total sample.
The most common age of onset for diabetes was between 6–10 years and 11–15 years, with each age group representing 38.9% of the cases. The mean age of diagnosis of T1DM was 8.87 years. A significant percentage of the children (79.6%) had been living with diabetes for 1–5 years, with an average duration of 3.85 years [Chart 1].
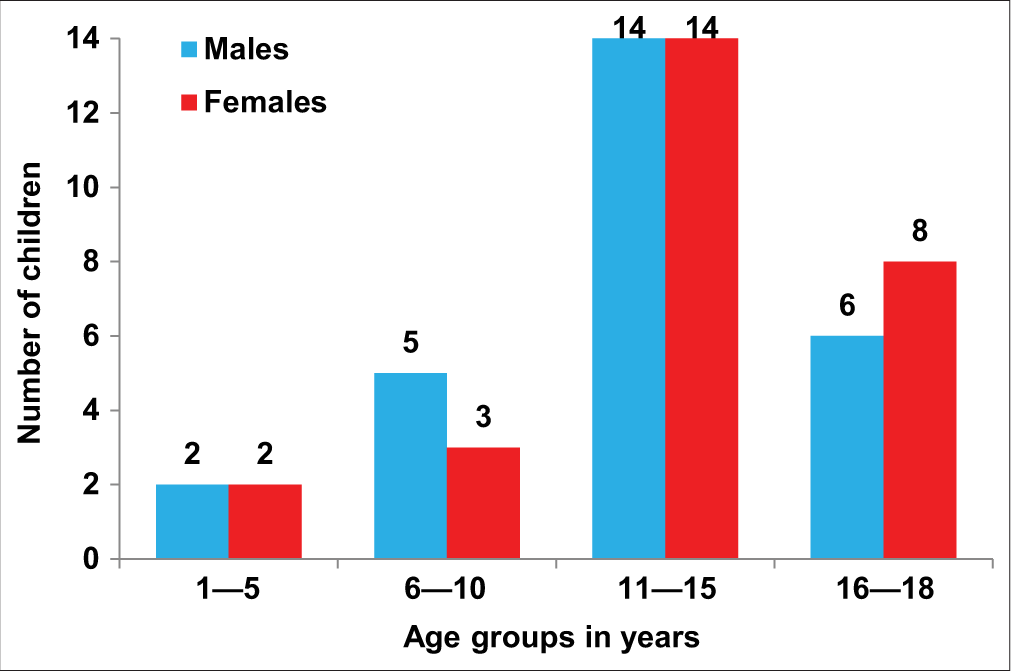
- Multiple bar diagram represents age and sex-wise distribution of children.
A significant majority (83.3%) of the children exhibited HbA1c levels ≥8.5%, reflecting inadequate glycaemic control. The mean HbA1c level across the group was 10.6% [Chart 2].
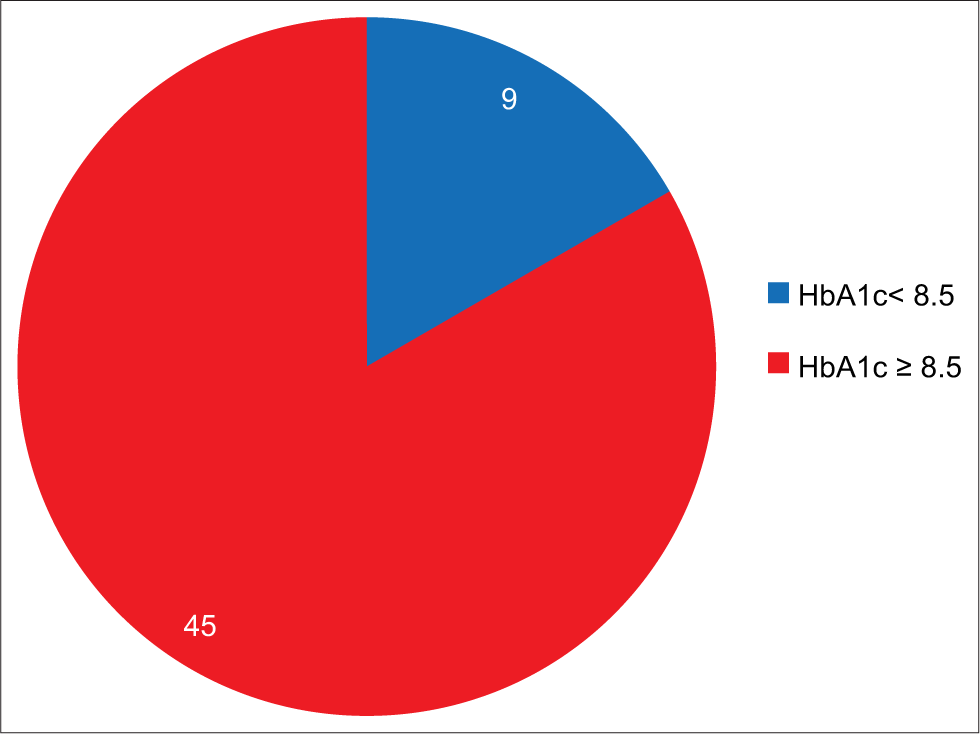
- Pie diagram represents level of glycated haemoglobin (HbA1c)-wise distribution.
No signs or symptoms of retinopathy were reported amongst the entire cohort. However, 3.7% of the participants were diagnosed with DR. The majority (96.3%) displayed normal findings upon fundoscopy [Table 2].
| Variable | Status | Number of children | Percentage |
|---|---|---|---|
| Signs and symptoms of retinopathy | Absent | 54 | 100.0 |
| Present | 0 | 0.0 | |
| Diabetic retinopathy | Absent | 52 | 96.3 |
| Present | 2 | 3.7 | |
| Fundoscopy findings | Normal | 52 | 96.3 |
| Abnormal | 2 | 3.7 |
A statistically significant relationship was identified between elevated HbA1c levels and the presence of DR (P = 0.011), with children exhibiting retinopathy showing a notably higher mean HbA1c of 13.60%. Furthermore, a significant correlation was established between the duration of diabetes and the occurrence of retinopathy (P = 0.023). Children with retinopathy had a longer average duration of diabetes (7.33 years) compared to those without retinopathy [Table 3].
| Comparison | Diabetic retinopathy | Mean±SD | 95% CI | P-value and significance |
|---|---|---|---|---|
| HbA1c Levels | Present | 13.60±3.48 | 1.34–6.44 | P=0.011, S |
| Absent | 10.38±2.25 | |||
| Duration of diabetes | Present | 7.33±3.21 | 0.46–5.96 | P=0.023, S |
| Absent | 3.58±2.21 |
SD: Standard deviation, CI: Confidence interval, HbA1c: Glycated haemoglobin, S: Significant
In conclusion, the study indicates that while the prevalence of DR in children with T1DM is relatively low, poor glycaemic control and longer diabetes duration are significantly associated with the development of DR.
DISCUSSION
In this cross-sectional study of 54 patients with T1DM, we examined the impact of glycaemic control and diabetes duration on the prevalence of DR over 18 months. The study found a 3.7% prevalence of DR, with significant associations between higher HbA1c levels and longer diabetes duration. Our cohort was evenly split by gender, with 27 males and 27 females, contrasting with other studies such as those by Ferm et al.,[4] Shibeshi et al.[2] and Porter et al.,[6], where as Rajguru et al.[7] had male prevalence, which reported a higher female prevalence [Table 4].
| Study | Male (%) | Female (%) | Male-to-female ratio (M) |
|---|---|---|---|
| Ferm et al., 2018[4] | 47.1 | 52.9 | 1:1.12 |
| Shibeshi et al., 2015[2] | 45.3 | 54.7 | 1:1.20 |
| Porter et al., 2018[6] | 44.3 | 55.7 | 1:1.25 |
| Rajguru et al., 2021[7] | 56 | 44 | 1:0.96 |
| Present study | 50 | 50 | 1:1 |
TIDM: Type 1 diabetes mellitus, HbA1c: Glycated haemoglobin
The mean age diagnosis of diabetes in our study was 8.87 years, aligning closely with Ferm et al.[4] findings but lower than the mean ages reported by Zabeen et al.[8] and Shibeshi et al.[2] The mean duration of diabetes was 3.85 years, which is shorter compared to Ferm et al.[4] and Shibeshi et al.[2] findings [Table 5].
| Study | Mean age at diagnosis (Years) | Mean duration of diabetes (Years) |
|---|---|---|
| Ferm et al., 2018[4] | 9.1 | 6.7 |
| Shibeshi et al., 2015[2] | 14.2 | 8 |
| Porter et al., 2018[6] | 11.5 | 4.1 |
| Zabeen et al., 2017[8] | 12.0 | – |
| Rajguru et al., 2021[7] | – | 4.65 |
| Present Study | 8.87 | 3.85 |
T1DM: Type 1 diabetes mellitus
This study observed a mean HbA1c of 10.6%, reflecting poorer glycaemic control relative to other studies like those by Ferm et al.,[4] Zabeen et al.,[8] Porter et al.[6] and Strul et al.[9] [Table 6].
| Study | Mean HbA1c (%) | Mean HbA1c in DR patients (%) | Mean duration of diabetes in DR patients (Years) | Percentage of DR | P-value (DR) |
|---|---|---|---|---|---|
| Ferm et al., 2018[4] | 9.75 | 10.3 | 9.4 | 3.5 | <0.01 |
| Zabeen et al., 2017[8] | 9.35 | 9.6 | 7.6 | 6.6 | 0.013 |
| Porter et al., 2018[6] | 8.65 | 9.8 | 10.4 | 3.8 | 0.45 |
| Strul et al., 2019[9] | 9.45 | 10.2 | 11 | 6.0 | <0.001 |
| Present Study | 10.6 | 13.6 | 7.3 | 3.7 | 0.023 |
T1DM: Type 1 diabetes mellitus, DR: Diabetic retinopathy, HbA1c: Glycated haemoglobin
In patients with DR, the mean HbA1c was significantly higher at 13.6%, a result consistent with Ferm et al.[4] and Porter et al.[6] studies. The mean duration of DM amongst these patients was 7.3 years, which aligns with Zabeen et al.[8] and indicates that both extended diabetes duration and elevated HbA1c levels are significant risk factors for DR. These findings emphasise the critical role of maintaining stringent glycaemic control to mitigate the risk of retinopathy in paediatric T1DM patients.
Limitation of the study
Single centre study and relatively small sample size.
The cases were not monitored over an extended period to evaluate the progression of DR.
CONCLUSION
The current study demonstrates a relatively low incidence of DR amongst children with diabetes. It underscores the significance of diabetes duration and HbA1c levels as contributing factors in Indian paediatric patients. Optimal glycaemic control is highlighted as crucial in mitigating the onset and progression of DR in young diabetics. Given the chronic nature of diabetes and the heightened risk of DR with prolonged disease duration, ensuring stringent glycaemic control is imperative as the primary and most effective measure to prevent or delay retinal complications. In addition to counselling for improved diabetes management, both young patients and their caregivers should be educated about the risks associated with DR and its potential vision-threatening consequences. Healthcare institutions and governmental bodies are encouraged to initiate extensive educational campaigns and screening initiatives, particularly amongst minority groups and rural populations.
Ethical approval
The research/study was approved by the Institutional Review Board at Mahadevappa Rampure Medical College Kalaburagi, number 202207102, dated 27th July, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Sharanagouda Patil is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Standards of medical care in diabetes. 2023. Available from: https://www.diabetes.org/standards-of-care [Last accessed 2024 Oct 23]
- [Google Scholar]
- Incidence and prevalence of diabetic retinopathy among children with type 1 diabetes: A review of the literature from Ethiopia. Ethiop J Health Sci. 2015;25:11-9.
- [Google Scholar]
- Global report on diabetes. 2021. Available from: https://www.who.int/publications/i/item/9789240066620 [Last accessed 2024 Oct 23]
- [Google Scholar]
- Gender differences in type 1 diabetes in youth: A review of current literature. Diabetes Res Clin Pract. 2018;142:200-11.
- [Google Scholar]
- Epidemiology of diabetic retinopathy in children with type 1 diabetes mellitus: A systematic review. Pediatr Diabetes. 2019;20:515-22.
- [Google Scholar]
- The relationship between glycemic control and retinopathy in children with type 1 diabetes: A longitudinal study. J Pediatr Endocrinol Metab. 2018;31:859-67.
- [Google Scholar]
- Gender differences and age-related variations in type 1 diabetes: A study from Rajasthan, India. Diabetes Res Clin Pract. 2021;173:108674.
- [Google Scholar]
- Mean age of onset and duration of diabetes among children with type 1 diabetes: A comparative study. Int J Diabetes Dev Countries. 2017;37:292-9.
- [Google Scholar]
- Glycemic control and diabetic retinopathy in adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2019;32:171-8.
- [Google Scholar]






