Translate this page into:
Traumatic brain injury unmasking Vitamin B12 deficiency in an infant with long-term follow-up
*Corresponding author: Vykuntaraju K. Gowda, Department of Pediatric Neurology, Indira Gandhi Institute of Child Health, Bengaluru, Karnataka, India. drknvraju08@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gowda VK, Shankar RT, Challa VR, Srinivasan VM. Traumatic brain injury unmasking Vitamin B12 deficiency in an infant with long-term follow-up. Karnataka Paediatr J. doi: 10.25259/KPJ_60_2023
Abstract
Falls are very common in infancy and toddler age group. We are presenting a case of insignificant fall from the cot causing severe neurological problems in an infant due to previous underlying relatively asymptomatic vitamin B12 deficiency. A six-month-old female infant presented with a fall from a cot followed by altered sensorium, vomiting, right focal seizures, and right sided weakness. On examination, a low Glasgow coma scale (8/15), right sided weakness (MRC power of 3/5 in the right upper and lower limbs), with anaemia were noted. Investigations revealed left frontal contusion with haemorrhage, megaloblastic anaemia, and thrombocytopenia with low vitamin B12 level. The child improved with symptomatic management of raised intracranial pressure and injectable vitamin B12 supplements. Prompt intervention and appropriate treatment led to favourable outcomes in the infant, highlighting the importance of recognizing and addressing concomitant deficiencies in infants with TBI.
Keywords
Traumatic brain injury
Vitamin B12 deficiency
Infancy
Neurological manifestations
Haematological manifestations
INTRODUCTION
Traumatic brain injury (TBI) is a significant concern in infants, requiring prompt evaluation and management to prevent potential complications. In the Indian scenario, 20–30% of head injuries are seen in the paediatric population between ages 1 and 16 years.[1,2] Vitamin B12 deficiency is very common in infancy and can lead to both haematological and neurological manifestations. Neurological manifestations include global developmental delay, neuroregression, irritability, lethargy, excessive crying, involuntary movements such as tremors and changes in behaviour such as agitation or withdrawal.[3-5] Haematological manifestations of Vitamin B12 deficiency include megaloblastic anaemia and pancytopenia. We report a case of a 6-month-old female infant who suffered an insignificant fall from a cot, resulting in intracranial haemorrhage due to previously unrecognised thrombocytopenia secondary to Vitamin B12 deficiency.
CASE REPORT
A 6-month-old female infant was brought to the emergency room after an alleged history of falling from a cot with onset of vomiting and right focal seizures after three hours. On examination, her weight was 8 kg (0 to +1 Z score), and her head circumference was 42 cm (0 to −1 Z score). There was severe pallor and hypopigmented spar hair with knuckle hyperpigmentation. No external injuries were noted. Glasgow Coma Scale: 9/15, with equal and reactive pupils with a power of 3/5 (Medical Research Council [MRC] grade), was observed on the right side.
Laboratory investigations revealed anaemia-haemoglobin of 6.1 g/dL with mean corpuscular volume (MCV) of 106.7, thrombocytopenia (13 × 103/uL) and low levels of serum Vitamin B12 121.2 pg/mL (normal 211–911 pg/mL) and increased levels of serum homocysteine of 89.83 μmoL/L (normal 3–50 μmoL/L). Peripheral smear examination indicated microcytic hypochromic cells, elongated cells, a few macro ovalocytes and hyper-segmented neutrophils. Serum iron was 59.04 ug/dL (35–145 ug/dL), Unsaturated iron binding capacity (UIBC) was 321.10 ug/dL (135–392 ug/ dL), total iron-binding capacity (TIBC) was 380.14 ug/ dL (250–400 ug/dL), transferrin was 310.2 mg/dL (200– 360 mg/dL), transferrin saturation was 15.53% (20–50%) and serum ferritin of 173.2 ng/Ml (20–110 ng/mL). Liver and renal function tests, serum electrolytes and metabolic workup done were normal. An initial computed tomography scan brain showed a haemorrhage in the left frontal region measuring 12 × 15 mm. Electroencephalogram showed focal epileptiform discharges arising from the left frontal region. A follow-up magnetic resonance imaging (MRI) of the brain after one month of trauma revealed volume loss and altered signal intensity in the left frontal lobe [Figure 1a-c], suggestive of gliosis due to injury.
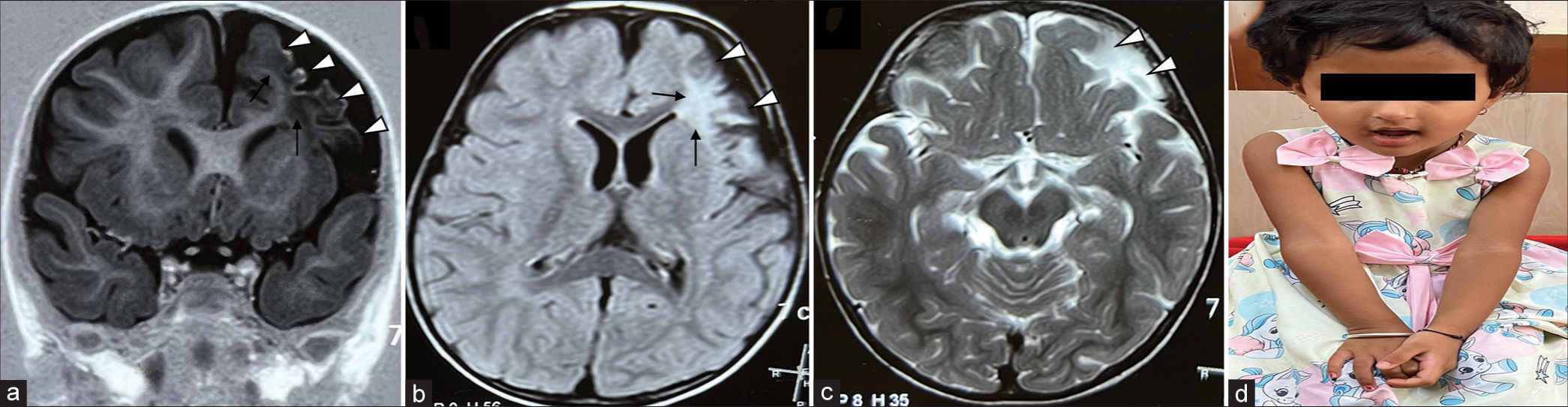
- (a) Magnetic resonance imaging brain with T1-weighted coronal (white arrow heads), (b) T2-weighted axial (white arrow heads) and (c) short tau inversion recovery axial sequences show loss of left frontal lobe volume (white arrow heads) with gliotic ischaemic areas (thin black arrows) in cortex and subcortical white matter regions, (d) Clinical photograph of the child during the last follow-up at three years showing mild residual weakness of the right upper limb.
Given the clinical findings of TBI and concurrent Vitamin B12 deficiency, she received intravenous levetiracetam and 3% sodium chloride and supportive care. To address her anaemia, she received packed red blood cells and IV Vitamin B12 (cyanocobalamin) at 1000 mcg/day for seven days followed by oral supplements continued for three months post-discharge. Due to persistent bicytopenia (severe anaemia and thrombocytopenia) during the prolonged hospital stay of 30 days, bone marrow aspiration was done, suggestive of megaloblastic anaemia.
Laboratory values post-treatment were Vitamin B12 of 11850 pg/mL (normal 211–911 pg/mL) and normalised levels of homocysteine of 16.68 μmoL/L (normal 3–50 μmoL/L). Her last follow-up at three years of age was found to have mild residual right upper and lower limb weakness [Figure 1d].
DISCUSSION
This case report highlights the unmasking of Vitamin B12 deficiency in an infant following TBI. The fall from the cot resulted in TBI, leading to symptoms such as vomiting and seizures. Despite the seemingly insignificant nature of the fall, the presence of hemiparesis, brain haemorrhage observed on MRI, as well as the co-occurrence of anaemia and thrombocytopenia, raised concerns of underlying Vitamin B12 deficiency. Initially, anaemia was attributed to being secondary to brain haemorrhage by trauma, but the cause of thrombocytopenia could not be explained, which prompted further investigation into Vitamin B12 deficiency along with clinical manifestations. Other causes of anaemia and thrombocytopenia, such as leukaemia, were ruled out after a bone marrow examination. Identification of low Vitamin B12 levels in the patient led to the recognition of an underlying deficiency, which has implications for neurological functioning.
Vitamin B12 deficiency is known to have neurological manifestations, including developmental delay/neuro regression, cognitive impairment in children, peripheral neuropathy and neuropsychiatric manifestations in the older age groups.[6] In addition to these effects, Vitamin B12 deficiency has also been associated with ischaemic stroke.[7] Studies have shown that Vitamin B12 deficiency can result in increased levels of homocysteine, an amino acid associated with an increased risk of vascular diseases, including stroke.[7] However, the exact mechanisms underlying the association between Vitamin B12 deficiency and worse outcomes in ischaemic stroke are still unknown.[7]
While this case report focuses on detailed clinical examination and analysis of investigations influencing the outcome, prompt intervention and appropriate treatment played crucial roles in achieving favourable outcomes. The findings from this case report underscore the importance of considering concomitant nutritional deficiencies in infants with TBI, as they can contribute to the clinical presentation and influence management strategies. The child is currently three years old, with regular follow-up and achieving age-appropriate milestones, weight of 10.6 kg (−2 to −3 Z score), head circumference of 46 cm (at −3 Z score) and mild paucity of movements on the right side. The limitation of the report is we do not have clinical and radiological images during initial admission.
CONCLUSION
TBI in infants can be complicated by underlying nutritional deficiencies, such as Vitamin B12 deficiency. This case report emphasises the significance of recognising and addressing concomitant deficiencies in infants with TBI, as they can impact clinical presentation and management strategies.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pediatric head injury In: Mahapatra AK, Kumar R, Kamal R, eds. Textbook of head injury. Delhi: Jaypee Publication; 2012. p. :180-90.
- [CrossRef] [Google Scholar]
- Traumatic brain injury. NIMHANS publication no. 61. Bangalore, India: NIMHANS. 2005. Available from: https://nimhans.ac.in/wp-content/uploads/2019/02/Traumatic-Brain-Injury_0.pdf [Last accessed on 2014 May 19]
- [Google Scholar]
- Neurologic findings of nutritional Vitamin B12 deficiency in children. Turk J Pediatr. 2010;52:17-21.
- [Google Scholar]
- Effects of Vitamin B12 and folate deficiency on brain development in children. Food Nutr Bull. 2008;29:S126-31.
- [CrossRef] [PubMed] [Google Scholar]
- Severe encephalopathy with epilepsy in an infant caused by subclinical maternal pernicious anemia: Case report and review of the literature. Eur J Pediatr. 2004;163:196-201.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993;270:2693-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of vitamin B12 deficiency on risk and outcome of ischemic stroke. Clin Biochem. 2023;118:110591.
- [CrossRef] [PubMed] [Google Scholar]







