Translate this page into:
A case of congenital multiple pancreatic cysts in a female child: A case report
*Corresponding author: Omar Abdulqader Ajaj, Department of Pediatric Surgery, College of Medicine, University of Anbar, Baghdad, Iraq. abd.o85@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Al-Bayati KF, Al-Hasnawi SM, Ajaj OA. A case of congenital multiple pancreatic cysts in a female child: A case report. Karnataka Paediatr J. 2024;39:57-9. doi: 10.25259/KPJ_56_2023
Abstract
Congenital pancreatic cysts are rare in the paediatric age group; they can be isolated or associated with other malformations. Prompt diagnosis and appropriate management are crucial to prevent complications. One and a half year old female presented with an abdominal mass. Surgical exploration revealed multiple cystic lesions occupying most of the abdominal and pelvic cavities originating from the pancreas. A complete surgical excision was done, and the histopathological examination confirmed the presence of islands of well-defined pancreatic tissue with scattered dilated ducts. True congenital pancreatic cysts are rare anomalies to occur, and there is female predominance for such conditions; early diagnosis and treatment are essential to prevent complications.
Keywords
Congenital cysts
Pancreatic cysts
True cysts
INTRODUCTION
Congenital pancreatic cysts are rarely reported in paediatric age group, and they can be an isolated condition or associated with other malformations.[1] Prompt diagnosis and appropriate management are crucial to prevent complications.[2] In our case report, this female baby has multiple pancreatic cysts as isolated anomalies managed by complete surgical excision. We think that the results of this study will be of utmost usefulness for the paediatric surgeon when considering congenital multiple pancreatic cysts in children.
CASE REPORT
One and a half years old baby female was referred to the paediatric surgery department in Child Welfare Teaching Hospital, complaining of abdominal distension for four months, which gradually increased in severity and was associated with decreased appetite and weight loss, but without vomiting or alteration in bowel habit. The patient had no history of fever or changes in sleep patterns. The child had no previous medical or surgical illnesses or admission to hospitals. Family history had nothing significant. During the examination, the baby was conscious, underweight, and pale, with moderate abdominal distension. A palpable abdominal mass was noticed on the right side of the abdomen; it was spherical mobile of about 3 × 4 cm in size.
A complete blood count revealed leukocytosis with normal haemoglobin, platelets, and morphology. All biochemistry investigations serum electrolytes, renal function, serum amylase and lipase, erythrocyte sedimentation rate [ESR], and alpha-fetoprotein were normal levels. Erect abdominal X-ray shows an abnormal soft-tissue shadow. Abdominal ultrasound showed a multiloculated cystic lesion in the entire abdomen and mainly the left upper abdominal quadrant, not related to any organ. Abdominal computed tomography scan with intravenous contrast showed multiloculated cystic lesions extended from the abdominal to the pelvic cavity, with a size of about 20 × 17 × 11 cm, with pressure effect on the abdominal and pelvic organs. There are no solid components and no significant enhancement [Figures 1a and b].
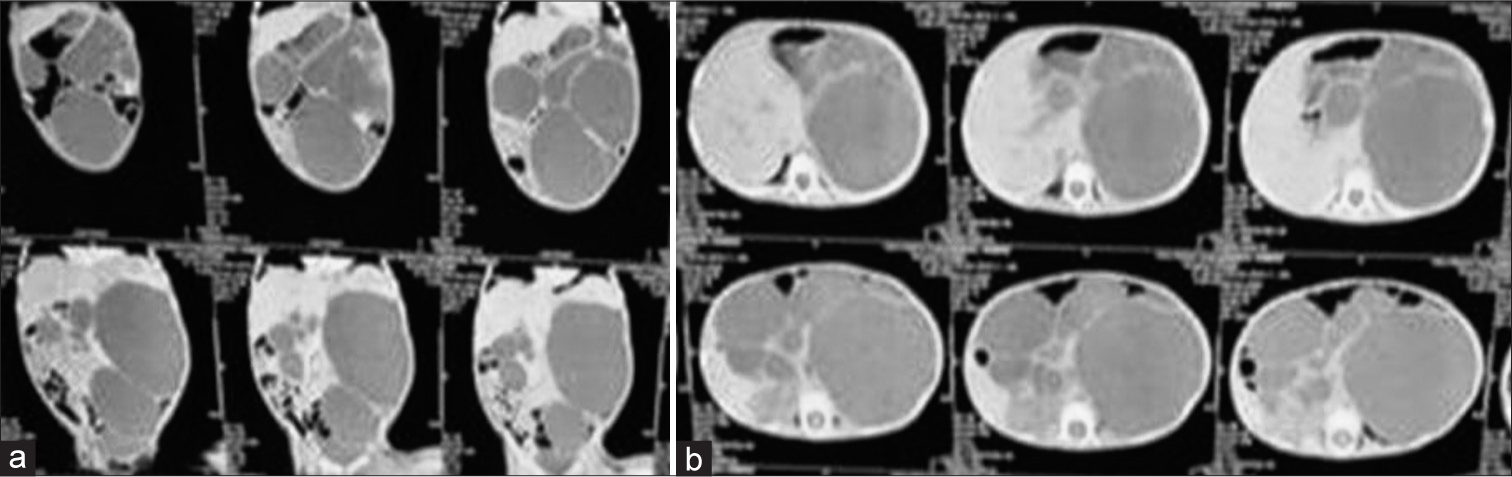
- (a and b) Computed tomography scan of the child showing multiple abdominal cysts.
Intra-operative findings show multiple pancreatic cysts of variable sizes. After delicate dissection and release of adhesion, the cysts were excised completely [Figures 2a and b, 3]. The cysts were sent for histopathological examination, which revealed multiple unilocular cysts with a wall thickness of 0.1 cm containing clear serous fluid. Cystic structures are lined by cuboidal and columnar glandular epithelium with thick fibrous walls containing islands of well-defined unremarkable pancreatic tissue and scattered with dilated ducts. No atypia or immature tissue could be seen. Picture consistent with true benign pancreatic cysts is shown in Figure 4. Post-operative follow-up for two years by clinical and abdominal ultrasound examination showed complete excision of cysts without recurrence. Written informed consent has been taken from the patient’s parent for publication. The Medical Ethics Committee of the University of Anbar, Anbar, Iraq, approved this study.
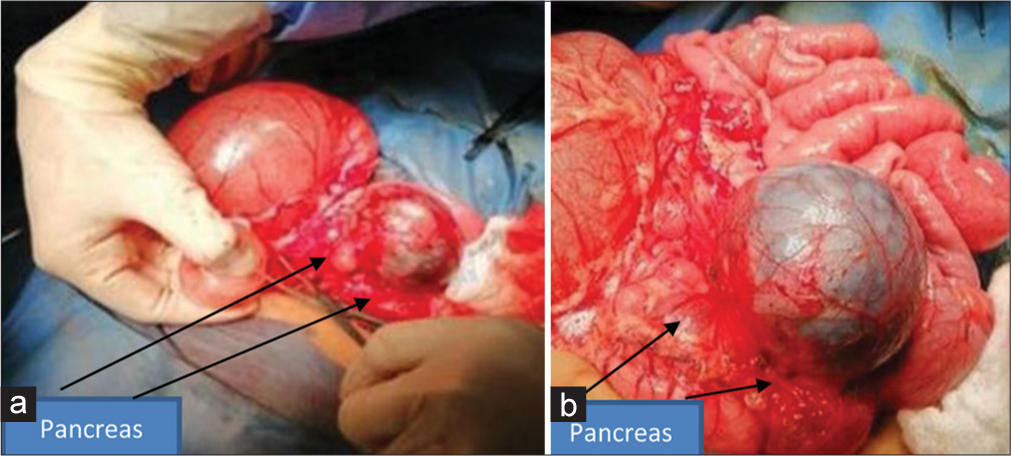
- (a and b) Operative picture shows the pancreas with multiple pancreatic cysts.

- Post-operative pancreatic cysts after excision with variable sizes.
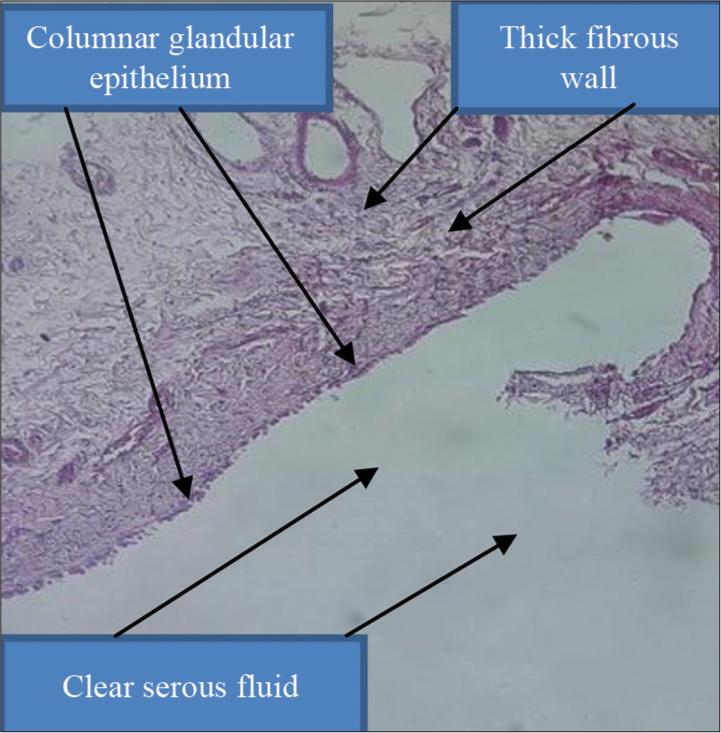
- Histopathological finding of pancreatic cyst.
DISCUSSION
Congenital pancreatic cysts in the paediatric age groups are rare. The incidence is <1% of all abdominal cysts.[1,2] Embryologically, true pancreatic cysts occur as a result of developmental anomalies related to the sequestration of primitive pancreatic ducts.[3] These cysts can be single or multiple. Congenital pancreatic cysts may or may not possess an epithelial lining or elevated serum amylase level; the presence of either supports the diagnosis.[3,4] There is female predominance for such conditions as in our case.[1]
Such pathology had been reported to be associated with other anomalies such as von Hippel-Lindau syndrome, polycystic kidney disease, Ivemark syndrome, and other conditions.[3,5,6] diagnosis can be made antenatally or postnatally, but prenatal diagnosis is extremely rare.[1,7,8] Patient may be asymptomatic or have abdominal mass with or without abdominal distension. Pressure symptoms are vomiting and jaundice due to compression on the stomach and biliary tree, respectively.[9,10]
Early diagnosis and treatments are essential to prevent the development of complications such as infection, cyst rupture, peritonitis, and pancreatitis.[4] The latter results either from congenital anomalies of the duct system or from visceral compression by the cyst.[3,11] It may be difficult to establish the diagnosis by depending on imaging studies, and the differential diagnosis may include choledochal cyst, lymphatic malformations, omental or mesenteric cyst or enteral duplications anomalies. Endoscopic retrograde cholangiopancreatography is useful to rule out communication with the pancreatic duct and biliary tree.[6]
CONCLUSION
We observed that the true congenital pancreatic cysts are rare anomalies with female predominance. Early diagnosis and treatment are essential to prevent complications.
Ethical approval
This research/study was approved by the Ethics Committee of the University of Anbar, and the reference number 211 dated 7th September 2023.
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Congenital cyst of the pancreas. J Pediatr Surg. 1993;28:1570-1.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal Diagnosis of giant congenital pancreatic cyst of a neonate. AJR Am J Roentgenol. 2000;175:1408-10.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal detection of a congenital pancreatic cyst and BeckwithWiedemann syndrome. Prenat Diagn. 1997;17:276-80.
- [CrossRef] [Google Scholar]
- Congenital pancreatic cysts in children. J Pediatr Surg. 2003;38:1080-2.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic detection of congenital pancreatic cysts in the newborn: Report of a case and review of the literature. Pediatr Radiol. 1990;20:488-90.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital true pancreatic cyst detected prenatally in neonate: A case report. J Pediatr Surg. 2007;42:E27-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pancreatic cyst in the newborn; a case report. Ann Surg. 1959;149:576-81.
- [CrossRef] [PubMed] [Google Scholar]
- Obstruction of the common bile duct in the newborn by a pancreatic cyst. Lancet. 1964;84:204-5.
- [Google Scholar]
- Pancreatic cyst arising from occlusion of the pancreatic duct. Pediatr Surg Int. 2007;23:903-5.
- [CrossRef] [PubMed] [Google Scholar]






