Translate this page into:
Congenital heart disease in children with acute lower respiratory tract infection
*Corresponding author: Mohammed Rabbani, Department of Paediatrics, Jagadguru Sri Shivarathreeshwara Medical College, JSS Academy of Higher Education and Research, Mysuru, Karnataka, India. mohammedrabbani1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rabbani M, Rajani HS. Congenital heart disease in children with acute lower respiratory tract infection. Karnataka Paediatr J. doi: 10.25259/KPJ_53_2024
Abstract
Objectives:
The objective of this study was to study the frequency of CHD among children aged 1 month to 12 years with ALRTIs at a tertiary care hospital in Mysuru.
Material and Methods:
This is a cross-sectional observational study that was conducted at a tertiary care hospital for 18 months (July 2022 to January 2024) to assess the frequency of CHD in children aged 1 month to 12 years with ALRTI. The sample size of 175 was calculated by taking 13% as the prevalence of CHD in children with pneumonia. Children with ALRTI and already diagnosed CHD cases with ALRTI were included in the study. Consecutive sampling was done. The patient underwent clinical evaluation and chest X-rays to diagnose ALRTI and echocardiography was done to identify CHD, and data on clinical outcomes were collected. Routine investigations were done and treatments were given as per hospital protocols. Outcome measures included hospital and paediatric intensive care unit stay duration, ventilator support needs and pneumonia resolution.
Results:
This study showed the prevalence of CHD in children with ALRTI to be 16.6%. Recurrent pneumonia occurred in 20.7% of children with CHD, compared to 6.8% without CHD, showing a significant association between CHD and recurrent pneumonia (Chi-square test, P = 0.03). CHD prevalence was 16.4% among children with pneumonia and 37.5% with recurrent pneumonia, which suggests that there is an increased prevalence of CHD in more severe or recurrent pneumonia cases. In addition, 27.6% of children with CHD developed congestive cardiac failure (CCF), compared to 4.8% without CHD, indicating a significant association between CHD and CCF (Chi-square test, P = 0.001).
Conclusion:
The present study demonstrates a strong relationship between CHD and lower respiratory tract infections (ALRTI) in children between 1 month and 12 years of age. The prevalence of CHD among children with ALRTI is 16.6%, and these children were at higher risk of developing CCF.
Keywords
Acute lower respiratory tract infection
Community-acquired pneumonia
Congenital heart disease
Recurrent pneumonia
INTRODUCTION
Acute lower respiratory tract infection (ALRTI)/bronchopneumonia is the most common cause of death in children under 5 years of age. Most cases of ALRTI in the world occur in developing countries. ALRTI results in 1.9 million childhood deaths per year in developing countries, and 20% of these deaths are from India.[1]
Several predisposing factors for ALRTI have been identified. Among them, severe acute malnutrition, immunodeficiency and congenital heart disease (CHD) are common. Children with CHD are more vulnerable to ALRTI due to anatomical defect that causes hemodynamic disturbances in the pulmonary circulation. They are at increased risk of morbidity as anatomic cardiac lesions can worsen an already compromised respiratory status.
The incidence of CHD in the general population is about 1% and varies from 4/1000 to 50/1000 live births. In India, the prevalence of CHD was found to be 2.25–5.2/1000 children.[1]
Ventricular septal defect (VSD), patent ductus arteriosus (PDA) and atrioventricular septal defect are the common acyanotic CHD with the left to right shunting of blood, pulmonary overcirculation, pulmonary oedema and congestive cardiac failure (CCF) which predispose to ALRTI. Truncus arteriosus and total anomalous pulmonary venous return are examples of cyanotic CHD that can predispose to ALRTI.
Early and accurate diagnosis of CHD in children presenting under the disguise of lower respiratory tract infection (LRTI) requires a systematic approach including detailed medical history collection and thorough clinical examination and investigations. The association of severity of ALRTI, CHD and CCF requires a multidisciplinary approach to prevent major cardiac and respiratory complications.
Early detection and appropriate management of CHDs can provide a child ample time for catch-up growth, reduce the morbidity and mortality risk associated with each episode of LRTI, significantly reduce the financial burden on the family and prevent long-term morbidities.
Very few studies have been conducted to evaluate the frequency of CHD in children with the first episode of ALRTIs.[2]
Identifying features that predict underlying CHD and outcome in these children with ALRTI at the very first episode will thus be helpful in preventing persistent or recurrent infections and must have a management plan accordingly. In this study, the primary aim is to assess the frequency of CHD in children from 1 month up to 12 years of age with ALRTI.
Objectives of the study
Primary objective
The objective of this study was to study the frequency of CHD in children between the age group of 1 month to 12 years with ALRTI in a tertiary care hospital in Mysuru.
Secondary objective
The objective of this study was to study the clinical characteristics and outcomes of ALRTI in children with or without CHD.
MATERIAL AND METHODS
Study design
This was a cross-sectional (observational) study.
Study duration
This study was 18 months from July 2022 to January 2024.
Sampling technique
Consecutive sampling was employed.
Sample size calculation
The sample size was calculated based on previous literature[1,2], which reported a prevalence of CHD in children with pneumonia to be 13%. With a precision of 5% and a 95% confidence interval, a sample size of approximately 175 children was required.
Study setting and method of data collection
Study design and location
This study is a cross-sectional observational study conducted at Tertiary Care Hospital, Karnataka.
Ethical clearance for the study was obtained from the Institutional Ethical Committee.
Consent process
Before enrolling in the study, written informed consent was secured from each child’s parent or legal guardian.
Inclusion criteria
All cases of ALRTI in children aged 1 month to 12 years who were admitted to the hospital.
Exclusion criteria
Children older than 12 years.
Children whose parents or legal guardians did not give consent.
Clinical evaluation
Each patient underwent a thorough clinical evaluation, with findings meticulously recorded.
Operational definitions
ALRTI
Defined as symptoms of fever, cough and tachypnoea as per the World Health Organization criteria:
0–2 months: Respiratory rate >60 cycles/min
2–12 months: Respiratory rate >50 cycles/min
12–59 months: Respiratory rate >40 cycles/min
>60 months: Respiratory rate >30 cycles/min
Additional signs include dyspnoea, chest in drawing, nasal flaring and with or without X-ray confirming LRTI.[1,3]
Pneumonia
Diagnosed based on typical history, physical findings (cough, chest wall in-drawing, difficulty breathing, tachypnoea and fever), blood investigations and chest radiography showing lobar or bronchopneumonia infiltrates in one or both lungs.
The most sensitive and specific clinical sign is tachypnoea, with auscultatory features being less sensitive.[1]
Recurrent pneumonia
Defined as at least two episodes of pneumonia in 1 year or three episodes over any period. Complete recovery with radiological clearance is expected between episodes.[4]
Persistent pneumonia
Defined as the persistence of symptoms (cough, tachypnoea and fever with or without chest retractions) and X-ray suggestive of LRTI in a child for more than a month, in spite of giving a 10-days of antibiotics.[4]
Heart failure
Diagnosed based on the following criteria:
Tachycardia: Heart rate more than 160 beats/min in infants, 140 beats/min in 2-year-olds, 120 beats/min in 4-year-olds and 100 beats/min in children older than 6 years. An acceptance of 10 beats/min for every 1°C rise in temperature is taken.
Tachypnoea: Respiratory rates more than 60 cycles/min in newborns, 40 cycles/min in children aged 28 days to 5 years, 28 cycles/min in those aged 5–10 years and 25 cycles/min in >10 years.
Cardiomegaly: Computed tomography ratio is more than 60% in children <5 years, or more than 50% in >5 years.
Tender hepatomegaly.[2]
A diagnosis of congestive heart failure is made if three of the above criteria are met.
Radiological and echocardiographic assessment
Each patient underwent a chest X-ray to diagnose pneumonia. X-ray was interpreted by a radiologist, with pneumonia confirmed when radiographic findings were positive.
Transthoracic 2D and Doppler echocardiography were performed on all ALRTI cases by a heart specialist or echo technicians with experience. CHD identified was documented.
Routine investigations and treatment
All other routine investigations were conducted according to hospital protocol.
Patients were treated following hospital protocols.
Outcome measures
Data were collected on several parameters, including duration of hospital stay, duration of paediatric intensive care unit (PICU) stay, need for ventilator support and clinical outcomes.
Resolution of pneumonia was determined based on normalisation of respiratory rate, vanishing chest findings and X-ray showing resolution.
Data collection tool
Information was systematically recorded using a structured pro forma. The following algorithm outlines the study methodology:
Study assessment of endpoints
The primary endpoint was to know the frequency of CHD in children under 12 years of age with ALRTI in a tertiary care hospital setting.
In addition, the study evaluated the clinical characteristics and outcomes of these children [Figure 1].
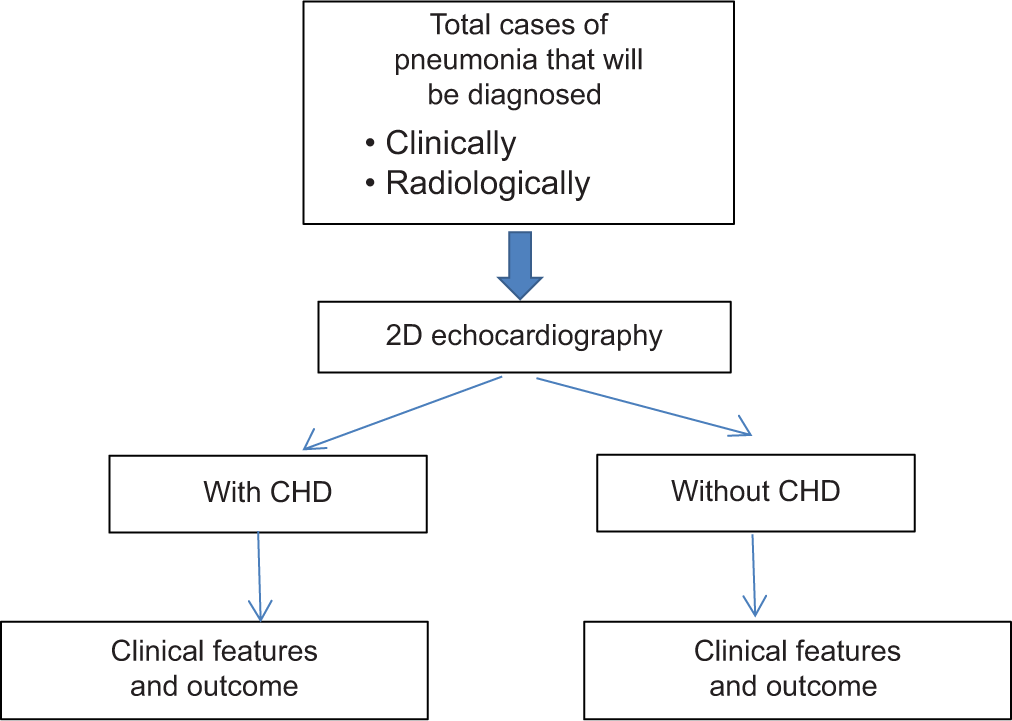
- Study flow chart. CHD: Congenital heart disease
Study conduct
Consent was taken from parents or legal guardians of the children, children were selected based on the inclusion criteria mentioned above.
History taking and clinical examination were done and findings were put in the predesigned pro forma.
Chest X-rays and ECHO were done on the children who were diagnosed with LRTI.
The outcomes of these children with ALRTI, with or without CHD, were systematically recorded.
Data analysis
All collected data were entered into Microsoft Excel and subsequently analysed using the Statistical Package for the Social Sciences Version 22 (Licensed to the Institution).
P < 0.05 was considered statistically significant.
RESULTS
Age distribution of the study population
The age distribution of the 175 children is shown in Figure 2

- Bar graph demonstrates the distribution of study population by age in months. Most of the children were <12 months old, which is 62.3% of the total population. Children between 13 and 60 months were 26.9%, children more than 61 months were 10.9%.
Findings
Most children (109; 62.3%) were <12 months old.
Children aged between 13 and 60 months accounted for 47 (26.9%), and those above 61 months were 19 (10.9%).
The mean age was 22.36 months (standard deviation ± 30.93), reflecting a wide age range.
The median age fell in the <12 months category, as calculated using cumulative frequency.
Gender distribution
The gender distribution is presented in Figure 3.

- Pie chart demonstrates the gender distribution among the study group. Out of 175 children in the study, 65.7% were male, and 34.3% were female.
Findings
Of the 175 children, 115 (65.7%) were male, and 60 (34.3%) were female.
A higher prevalence of male children was observed, with males being nearly twice as many as females.
Distribution based on pneumonia
The distribution of pneumonia among the study population.
Findings
Pneumonia was diagnosed in 159 (90.9%) of the children, making it the predominant ALRTI.
Other ALRTIs, such as bronchiolitis and wheeze-associated LRTIs, accounted for only 16 (9.1%) of the cases.
Prevalence of recurrent pneumonia
Findings
Recurrent pneumonia was observed in 16 (9.1%) children, while 159 (90.9%) did not experience repeated episodes.
Although recurrent pneumonia was less common, it remains a significant concern for children with ALRTI.
Prevalence of CHD
The prevalence of CHD in the study population is shown in Figure 4.
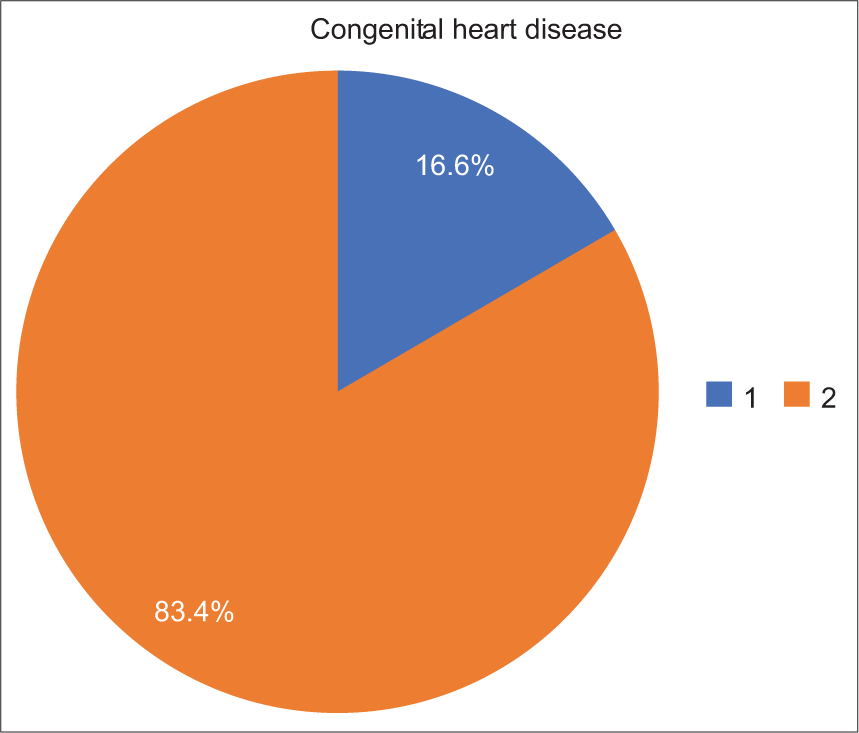
- Pie chart shows the presence of congenital heart disease (CHD) in the study children. CHD was present in 16.6% of the children, while 83.4% did not have CHD.
Findings
CHD was present in 29 (16.6%) children, whereas 146 (83.4%) did not have CHD.
This underscores the co-occurrence of CHD in a significant portion of children with ALRTI.
Prevalence of CCF
The distribution of CCF among the children is shown
Findings
CCF was diagnosed in 15 (8.6%) children, while 160 (91.4%) did not exhibit this condition.
Although CCF was less prevalent, it was predominantly observed in children with CHD and pneumonia.
Frequency of pneumonia in children with and without CHD
The frequency of pneumonia among children with and without CHD is shown in Figure 5.
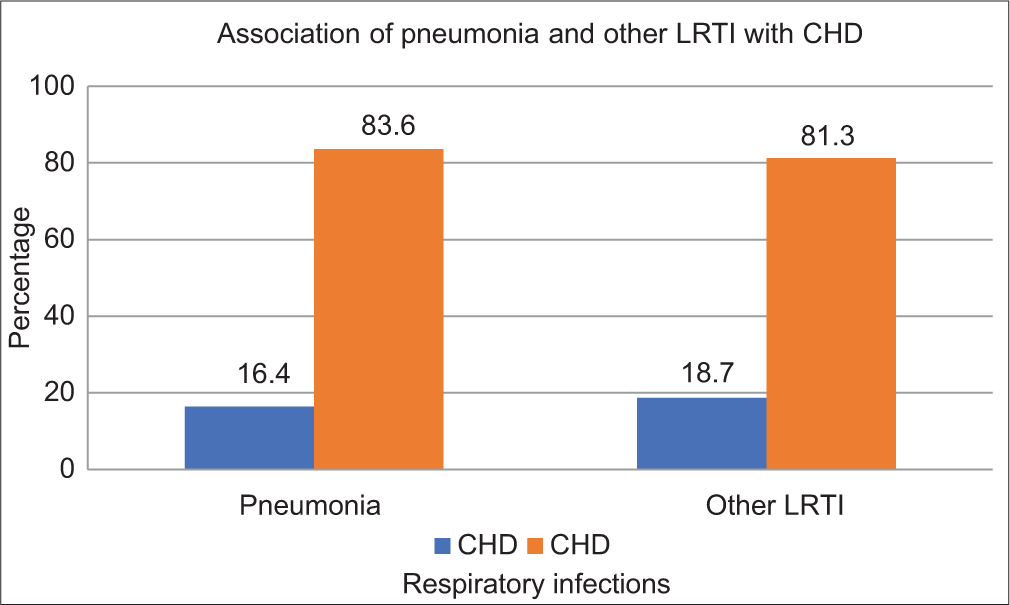
- Bar graph demonstrates the frequency of pneumonia in congenital heart disease (CHD). It shows 89.7% of children with CHD had pneumonia, 91.1% of those without CHD had pneumonia. The statistical analysis (Fisher’s Exact test) shows no significant association (P = 1), which suggests that CHD is not significantly associated with the incidence of pneumonia.
Findings
Of the 29 children with CHD, 26 (89.7%) had pneumonia.
Among the 146 children without CHD, 133 (91.1%) had pneumonia.
Fisher’s Exact test yielded a P-value of 1.0, indicating no statistically significant association between CHD and the incidence of pneumonia.
Association between CHD and recurrent pneumonia
The relationship between CHD and recurrent pneumonia is summarised in Figure 6.
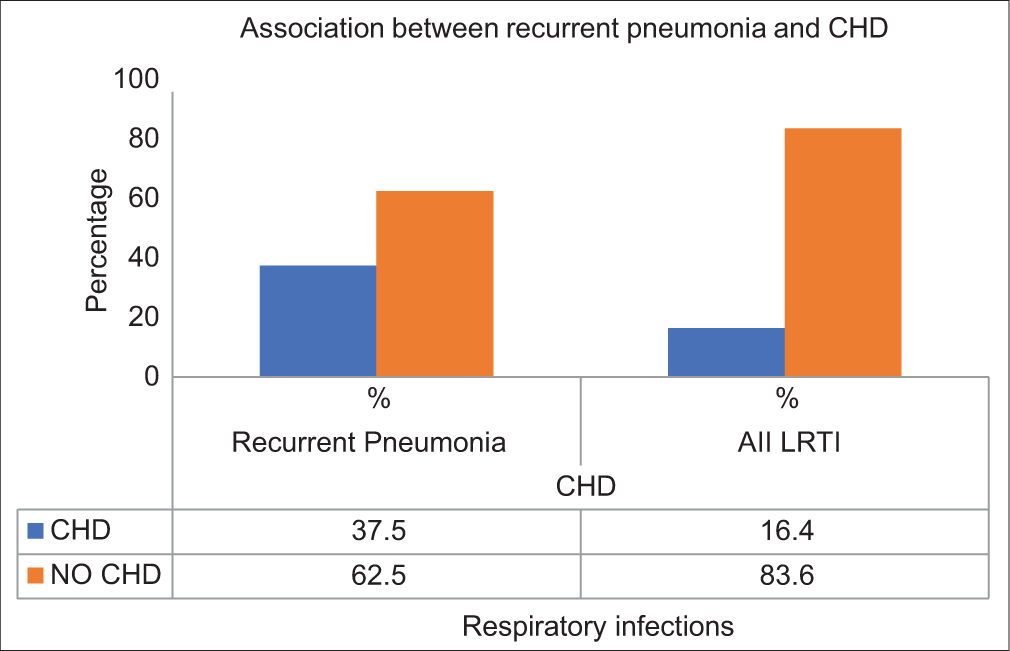
- Bar graph explains the relationship between congenital heart disease (CHD) and recurrent pneumonia. It shows that 20.7% of children with CHD had recurrent pneumonia, compared to 6.8% of those without CHD. The Chi-square test indicates a statistically significant association between CHD and recurrent pneumonia (P = 0.03), which suggests that children with CHD are more likely to develop recurrent pneumonia.
Findings
Recurrent pneumonia was observed in 6 (20.7%) of the 29 children with CHD, compared to 10 (6.8%) of the 146 children without CHD.
Statistical analysis using the Chi-square test revealed a significant association (P = 0.03), suggesting that children with CHD are at a higher risk of developing recurrent pneumonia.
Prevalence of CHD in pneumonia and recurrent pneumonia
The prevalence of CHD among children with pneumonia and recurrent pneumonia is shown in Figure 7.
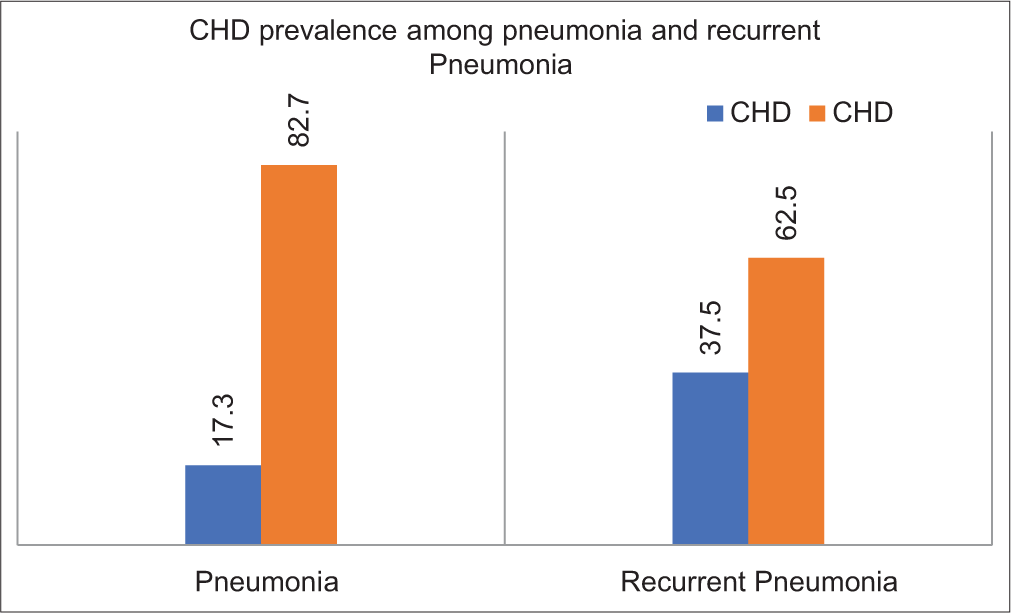
- Bar graph explains the prevalence of congenital heart disease (CHD) among children with pneumonia and recurrent pneumonia, CHD was present in 16.4% of children with pneumonia and 37.5% with recurrent pneumonia. This shows higher prevalence of CHD in recurrent pneumonia than in the first pneumonia episode, which suggests that CHD can lead to more repeated respiratory tract infection leading to recurrent pneumonia.
Findings
CHD was present in 26 (16.4%) of the 159 children with pneumonia.
Among the 16 children with recurrent pneumonia, 6 (37.5%) had CHD.
This indicates a higher prevalence of CHD in recurrent pneumonia cases, suggesting that CHD may predispose children to repeated respiratory tract infections.
Association between CHD and CCF in pneumonia
The relationship between CHD and CCF in children with pneumonia is summarised in Figure 8.
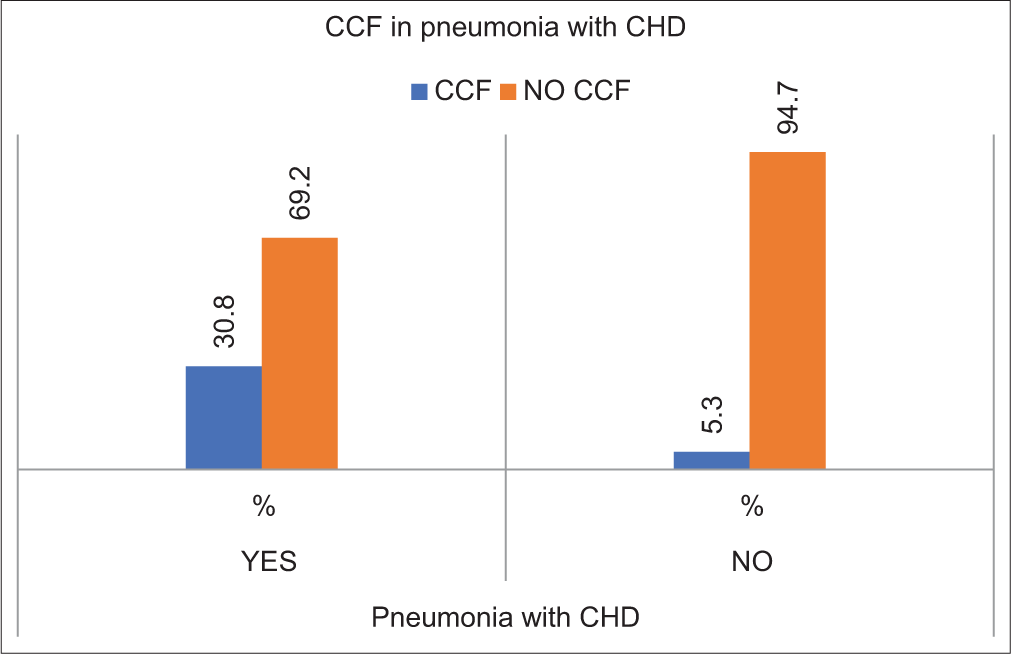
- Bar graph demonstrates the relationship between congenital heart disease (CHD) and Congestive cardiac failure (CCF) in children with pneumonia. CCF was seen in 30.8% of children with CHD, and 5.3% of those without CHD. The Chi-square test showed statistically significant association (P = 0.001), which suggests that CHD increases the chance of developing CCF in children with pneumonia.
Findings
Among the 26 children with CHD, 8 (30.8%) had CCF, compared to 7 (5.3%) of the 133 children without CHD.
The Chi-square test showed a statistically significant association (P = 0.001), suggesting that CHD significantly increases the risk of developing CCF in children with pneumonia.
Association between PICU admission and CHD in pneumonia
It shows that PICU admission was seen in 65.4% of children with CHD compared to 46.6% of children without CHD which was not statistically significant (P=0.09) [Figure 9].
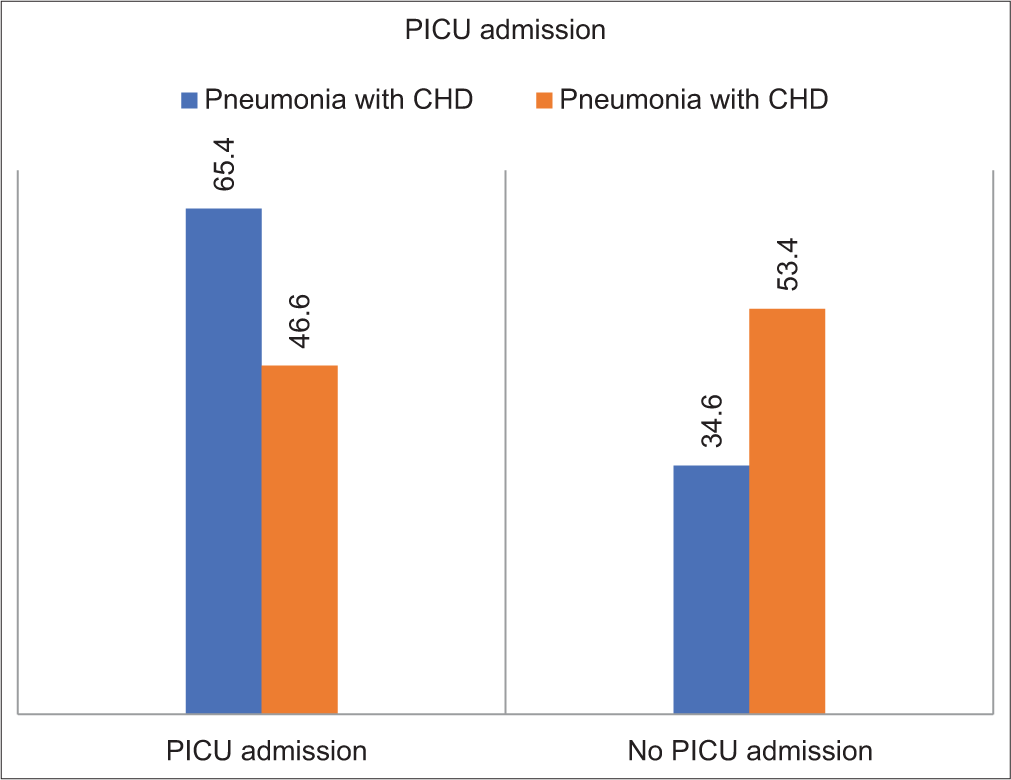
- Bar graph explains about the relationship between paediatric intensive care unit (PICU) admission and congenital heart disease (CHD) in children with pneumonia. It shows that PICU admission was seen in 65.4% of children with CHD compared to 46.6% of those without CHD. The Chi-square test does not show any statistically significant association (P = 0.09), which suggests that CHD had no significant influence in PICU admission in patients with pneumonia.
Findings
PICU admission was required for 17 (65.4%) children with CHD and 62 (46.6%) of those without CHD.
Although the percentage was higher in children with CHD, the Chi-square test revealed no statistically significant association (P = 0.09), indicating that CHD did not have a significant influence on PICU admissions.
Association between the need for ventilator support and CHD in pneumonia
Findings
Ventilator support was required in 4 (15.4%) of the 26 children with CHD, compared to 10 (7.6%) of the 133 children without CHD.
Fisher’s Exact test showed a statistically significant association (P = 0.002), indicating that children with CHD are more likely to require ventilator support when they develop pneumonia [Figure 10].
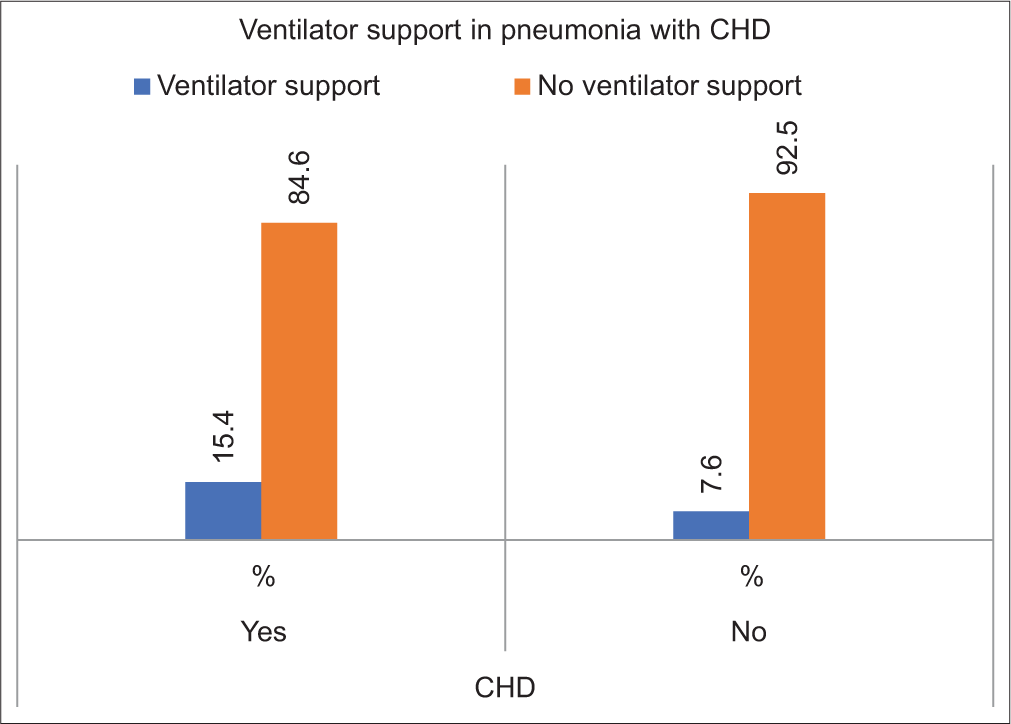
- Bar graph demonstrates the need for ventilator support in children with pneumonia and congenital heart disease (CHD). Ventilation requirement was seen in 15.4% of children with CHD and 7.6% without CHD. The Fisher’s Exact test showed statistically significant association (P = 0.002), which indicates that children with CHD are more likely to require ventilator support when they develop pneumonia.
Association between outcomes and CHD in pneumonia
Findings
Death occurred in 1 (3.8%) child with CHD and 5 (3.8%) children without CHD, showing no difference in mortality rates.
Improvement was noted in 18 (69.2%) children with CHD, compared to 122 (91.7%) of those without CHD.
A higher proportion of children with CHD (7; 26.9%) left against medical advice (LAMA) or were referred compared to 6 (4.5%) children without CHD.
Fisher’s Exact test demonstrated a statistically significant association (P = 0.002), suggesting poorer outcomes and higher non-compliance rates in children with CHD and pneumonia [Figure 11].

- Bar graph explains about the outcomes of pneumonia in children with and without congenital heart disease (CHD). It includes death, improvement and leaving against medical advice/referred. It shows death occurs in 3.8% of children with CHD. About 69.2% of children with CHD showed improvement compared to 91.7% without CHD, and 26.9% of children with CHD were either referred or left against medical advice compared to 4.5% without CHD. The Fisher’s Exact test shows a statistically significant association (P = 0.002), which indicates that CHD does not affect the outcome of pneumonia.
Type of CHD in children with pneumonia
Findings
The most commonly observed CHD type was atrial septal defect (ASD), found in 15 children (51.7% of the CHD cases).
PDA was documented in 7 cases (24.1%)
VSD accounted for 5 cases (17.2%)
Less frequently encountered CHD types included bicuspid aortic valve and cor triatriatum, each seen in 1 child (3.44%)
The prevalence of CHD types in the study was analysed using descriptive statistics
The high occurrence of ASD and PDA suggests a notable pattern in the population studied.
DISCUSSION
Age distribution
The present study showed that 62.3% of children are <12 months old, and the mean age is 22.36 months. This is similar to the findings of the other studies that we referred to, particularly the study done by Jat et al.[1] in 2021. In his study, the average age of children was reported as 9.94 months, with 77.5% of cases being < 1 year old. This suggests that there is a similar pattern of age distribution of children diagnosed with pneumonia across various studies.[5,6]
However, the percentage of children under 12 months in our study is lower than in the reference study by Jat et al.[1] It can be due to the primary focus on CHD in the study group, which could have caused higher mean age.
Gender distribution
Our study showed that 65.7% of the children were male and 34.3% were female, which indicates a higher chance of respiratory infections in males in the study group. This is similar to a study done by Jat et al.,[1] in 2021; they reported higher male proportions in children with pneumonia; males were 56.3% males compared to females who were 43.8%. This finding suggests that there is a higher chance of developing a respiratory infection in males compared to females.[5,7]
In contrast to our study, the study conducted by Izzati et al.[6] in 2019, Dr. Soetomo General Hospital in Surabaya found out that females were more prone to infection at 60.9% compared to males; only 39.1% of males developed respiratory tract infections among children with CHD. This difference could be due to different types of study populations or regional variations in gender susceptibility to respiratory infections.
Pneumonia
Our study showed that out of 175 cases of LRTI, 159 were pneumonia, which is around 90.0% of the study population; the rest were other LRTI cases, such as bronchiolitis and wheeze-associated lower respiratory tract infection. This shows that there is a high proportion of pneumonia cases present in our study which is almost equal to the total study population. This finding is similar to the other studies as well, in a study done by Yasmine et al.[7] in 2022, they found out that most of the children with CHD had pneumonia as a respiratory tract infection which is comparable to our study.
Our study is also comparable with a study done by Jat et al.[1] in 2021, their study shows pneumonia being the most common cause of admission among children with CHD.
Recurrent pneumonia
In our study, recurrent pneumonia was present in 9.1%. This finding is comparable with the study done by Jat et al.[1] in 2021, in their study, recurrent pneumonia was present in 20.6% of the children with CHD, which is slightly higher than our study, but both studies emphasise that there is an increased risk of recurrent pneumonia in children with CHD.
CHD
In our study, CHD was present in 16.6% of the children. This finding is comparable with the study done by Jat et al.[1] in 2021, where CHD was present in 12.5% of children with pneumonia. The small amount of difference could be due to specific population or regional factors in the studies.
CCF
Our study showed that CCF was present in 8.6% of the children; CCF usually presents with CHD. This finding is similar to the findings seen in the study by Jat et al.[1] in 2021, in their study, CCF was present in 27.5% of the children with pneumonia and CHD. The difference is due to the varied severity of CHD in the study population.
Another study which was done by Yasmine et al.,[7] in 2022, also noted that CCF was a major complication in children with acyanotic CHD, particularly those with conditions leading to pulmonary overcirculation. Our study has a lower proportion of CCF, which may be due to earlier interventions and different protocols for the management of CCF in our hospital.
Association of CHD with pneumonia
Our study has reported that there is no statistically significant association between CHD and pneumonia incidence (P = 1). This is similar to the findings of a study done by Jat et al.,[1] in their study also, the association between the two was insignificant. This tells us that even though CHD is prevalent in children with LRTI, it does not increase the risk of developing pneumonia.
Association of CHD with recurrent pneumonia
Our study showed a statistically significant association between CHD and recurrent pneumonia (P = 0.03), with 20.7% of children with CHD experiencing recurrent episodes. This finding is comparable with the study done by Yasmine et al.[7] in 2022, which also reported a higher risk of recurrent respiratory infections in children with acyanotic CHD.
The study by Jat et al.[1] in 2021 showed similar findings, which reported that there is high risk of development of recurrent pneumonia in patients with CHD.
Prevalence of CHD with pneumonia and recurrent pneumonia
Our study found that 16.4% of children with pneumonia had CHD, and 37.5% of those with recurrent pneumonia had CHD. This finding is similar to the findings from Jat et al.[1] in 2021, there study showed that 12.5% of children with pneumonia had CHD, and 55% of CHD cases were associated with the first episode of pneumonia.
Similarly, the study by Singh,[8] in 2017, showed a prevalence of 46.5 % of CHD in recurrent pneumonia, which is higher than our study
The study by Sadoh and Osarogiagbon[2] reported an 11.5% prevalence of CHD in the first episode of pneumonia, which is similar to our study.
The study by Harish and Kalyani[9] showed a 10% prevalence of CHD in pneumonia which is lower compared to our study [Table 1].
| S. No. | Name | Year of study | Cases | Age (years) | No. of children studied | Prevalence of CHD (%) |
Inference |
|---|---|---|---|---|---|---|---|
| 1. | Jat et al.[1] | 2022 | First episode recurrent pneumonia, persistent pneumonia |
Under five | 115 33 12 |
9.56 24.2 8.3 |
This study demonstrated a statistically significant prevalence of CHD in both pneumonia and recurrent pneumonia |
| 2. | Harish and Kalyani[9] | 2016 | Recurrent pneumonia | Under five | 40 | 10 | This study demonstrate lower prevalence of CHD than present study |
| 3. | Singh[8] | 2017 | Recurrent pneumonia | Under Twelve | 100 | 46.5 | This study demonstrate higher prevalence of CHD than present study |
| 4. | Present Study | 2022–2024 | LRTI (Pneumonia, Recurrent pneumonia) | Under twelve | 175 (159, 16) | 16.5 (16.4, 37.5) | The study showed statistically insignificant prevalence of CHD in pneumonia but significant in recurrent pneumonia |
LRTI: Lower respiratory tract infection, CHD: Congenital heart disease.
Association of CHD with CCF
In the present study, 27.6% of children with CHD developed CCF compared to 4.8% without CHD, this is a statistically significant association (P = 0.001). This finding is similar to the findings seen in the study done by Jat et al.[1] in 2021, in their study, 27.5% of children with pneumonia had CCF, and the majority (55%) of CHD cases were diagnosed with CCF.
In a study done by Nimdet and Techakehakij[10] in 2017, the prevalence of CCF was 10% which is lower than our study, whereas a study by Sadoh and Osarogiagbon,[2] in 2012, showed the prevalence of CCF to be 64% in children with pneumonia and CHD, which is higher than our study [Table 2].
| S. No. | Name | Year of study | Cases | Age (in years) |
No. children studied | Prevalence of CCF (%) | Inference |
|---|---|---|---|---|---|---|---|
| 1. | Jat et al.[1] | 2022 | Pneumonia with CHD Pneumonia without CHD |
Under five | 20 140 |
80 20 |
This study demonstrated a statistically significant association |
| 2. | Nimdet and Techakehakij et al.[10] | 2017 | Pneumonia | Under five | 135 | 10 | Study population showed 10% prevalence of CCF which is lower than current study. |
| 3. | Sadoh and Osarogiagbon[2] | 2012 | Pneumonia with CHD Pneumonia without CHD |
Under sixteen | 14 107 |
64 37 |
This study demonstrate higher prevalence than present study |
| 4. | Present Study | 2022–2024 | Pneumonia with CHD Pneumonia without CHD |
Under 12 | 26 133 |
30.8 5.3 |
Present study showed statistically significant association |
CHD: Congenital heart disease, CCF: Congestive cardiac failure
Association between CHD and CCF in pneumonia
Our study showed that 30.8% of children with CHD developed CCF in the context of pneumonia, compared to 5.3% without CHD, with a statistically significant association (P = 0.001). This is similar to findings seen in the study done by Jat et al.,[1] in 2021; they found that CCF was present in high proportion in children with pneumonia and CHD.
Similarly, the study by Yasmine et al.,[7] in 2022, showed that children with CHD, especially those with large VSDs, are at an increased risk of CCF when they develop pneumonia. It educates us regarding the importance of a multidisciplinary approach in the management of children with CHD and pneumonia.
Association between PICU admission and CHD in pneumonia
Our study showed that 65.4% of children with CHD required PICU admission for pneumonia, compared to 46.6% without CHD; this was statistically insignificant (P = 0.09). This is similar to the findings of the study by Jat et al.,[1] in 2021; in their study, a high proportion of the children who had CHD and severe pneumonia required an intensive care unit, highlighting the severity of their condition.
Yasmine et al.,[7] in 2020 also showed higher PICU admissions in children with CHD, particularly those with acyanotic defects like ASD, due to complications such as CCF. These findings suggest that while not all cases may require PICU care, children with CHD are at a higher risk of severe outcomes when hospitalised for pneumonia.
Association between the need for ventilator support and CHD in pneumonia
The present study showed that 15.4% of children with CHD required ventilator support due to pneumonia, compared to 7.6% of those without CHD; this is a statistically significant association (P = 0.002). This is similar to the findings from Jat et al.,[1] in 2021, where children with CHD were more likely to need mechanical ventilation due to severe respiratory distress.
Yasmine et al.,[7] in 2022, also showed similar findings that children with CHD, especially those with severe pulmonary congestion from acyanotic defects, frequently required ventilator support during respiratory infections. These findings show the critical role of ventilator support in managing severe pneumonia in children with CHD.
Association between outcome and CHD in pneumonia
In our study, 3.8% of children with CHD and pneumonia died, and 26.9% LAMA or were referred, compared to 3.8% and 4.5%, respectively, in children without CHD, with a statistically significant association (P = 0.002). It matches the findings of Jat et al.[1] in their study they noticed poor outcomes such as high mortality and complications then our study in children with CHD reported worse outcomes in children with CHD.
The study by Yasmine et al.[7] also noted that children with CHD had poor outcomes including higher mortality and longer hospital stays. This educates us regarding the importance of ICU management strategies to prevent severe outcomes.
Type of CHD in children with pneumonia
The present study showed the most common type of CHD being ASD and PDA; this is similar to the findings of the study by Yasmine et al.,[7] where acyanotic CHD, particularly ASD and VSD, was the most prevalent type.
Jat et al.[1] also showed similar findings, with VSD and PDA being the most common CHDs detected in children with pneumonia.
Limitations
The present study was done at a single centre; it limits the ability of the study to show authentic results for the broader paediatric population.
There are a few confounding variables, such as preexisting CHD and environmental factors, which could influence the prevalence of CHD and pneumonia.
Our study was cross-sectional; hence, it does not include long-term follow-up, which may fail to capture the complete association between CHD and LRTI.
In our study, we had taken the age limit to 12 years, which gave wide variations in results.
CONCLUSION
Our study demonstrates the significant relationship between CHD and ALRTIs/pneumonia in children between 1 month and 12 years of age. We found that the prevalence of CHD among children with pneumonia is 16.4%. Children in this study, who were affected by both pneumonia and CHD, are at higher risk of developing CCF and severe outcomes.
Acknowledgement:
I express my sincere thanks to Dr. H. Basavanagowdappa M.D., Principal, Dean and Professor of Medicine, Ethical Committee Chairman, for guiding, counselling and correcting me throughout the study period. I would also like to thank other members of Ethical Committee, for clearing my study. I appraise my gratefulness, admiration and regards for Dr. S. N. Prashanth M.D., Professor and Head of Department of Paediatrics, for his exquisite propositions and expert counsel during my study. I express my sincere thanks to my family especially my parents for their support and encouragement. I extend my sincere thanks to all my colleagues, my seniors and my juniors for their constant companionship and support throughout the course.
Last but not least, my heartfelt thanks to all the patients and volunteers who participated in this study and co-operated wholeheartedly.
Ethical approval:
The research/study approved by the Institutional Review Board at JSS academy of higher education and research, number JSS/MC/PG/IEC-59/2022-23, dated 26 August 2022.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship: Nil.
References
- Assessment of the prevalence of congenital heart disease in children with pneumonia in tertiary care hospital: A cross-sectional study. Ann Med Surg (Lond). 2022;73:103111.
- [CrossRef] [PubMed] [Google Scholar]
- Underlying congenital heart disease in Nigerian children with pneumonia. Afr Health Sci. 2013;13:607-12.
- [CrossRef] [PubMed] [Google Scholar]
- Revised WHO classification and treatment of pneumonia in children at health facilities: Evidence summaries. 2014. Geneva: World Health Organization; :26. Available from: https://iris.who.int/handle/10665/137319 [Last accessed on 2024 Jul 03]
- [Google Scholar]
- Persistent pneumonia: Underlying cause and outcome. Indian J Pediatr. 2009;76:1223-6.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of congenital heart disease in children with recurrent respiratory tract infection. Perinatology. 2016;17:89-94.
- [Google Scholar]
- Profile of children with congenital heart disease and upper respiratory tract infection in Dr. Soetomo General Hospital Surabaya period March 2018. JUXTA J Ilmiah Mahasiswa Kedokteran Univ Airlangga. 2019;10:57-9.
- [CrossRef] [Google Scholar]
- Incidence of respiratory tract infection in children with cyanotic and acyanotic congenital heart disease: A comparative study. JUXTA J Ilmiah Mahasiswa Kedokteran Univ Airlangga. 2022;13:62-6.
- [CrossRef] [Google Scholar]
- Incidence of congenital heart disease in children with recurrent respiratory tract infection in tertiary hospital. IOSR J Dent Med Sci. 2017;16:42-4.
- [Google Scholar]
- Study of prevalence of underlying congenital heart disease in children with recurrent respiratory tract infections. Perspect Med Res. 2017;5:20-3.
- [Google Scholar]
- Congestive heart failure in children with pneumonia and respiratory failure. Pediatr Int. 2017;59:258-64.
- [CrossRef] [PubMed] [Google Scholar]







