Translate this page into:
A non-invasive novel approach for managing digestive tract foreign body ingestion in children
*Corresponding author: Sayanthan Balasubramaniam, Department of Surgery, University of Jaffna, Jaffna, Sri Lanka. srisayan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sayanthan B, Sanjaya A, Ganeshrajah A, Thiruvarangan S. A non-invasive novel approach for managing digestive tract foreign body ingestion in children. Karnataka Paediatr J 2022;37:19-23.
Abstract
Objectives:
The phenomenon of foreign body ingestion (FB) is considered a common scenario in children’s tertiary care clinical settings. This study aimed to assess the sociodemographic factors of ingested FB, and its details and find the efficient clinical outcomes of a novel non-invasive interventional approach for removing FB in children.
Material and Methods:
This was a prospective study of 55 patients in a tertiary care centre, Sri Lanka for 1 year from 2019. The univariate, bivariate analysis, and the Chi-squared test were used to check the relationship between two categorical variables as this study dataset comprises more than 50 observations, where 5% was used as the significance level.
Results:
This study’s mean age was 5.18 ± 3.1 years and the median 5 years. The higher number of ingested FB was metal (88.5%) among this coin (33.3%) recorded the highest contribution and round shape was 62% whereas the ratio between sharp edge and none sharp edge was 1:4. A greater number of children both males (58.3%) and females (30.6%) were managed spontaneously to pass the FB through stool while vomiting (2.78%) was observed only in males. In comparison, the endoscopy removal cases were female (5.56%) and their mean age was 7.7 years.
Conclusion:
There are a number of studies that claim that the management of FB ingestion relatively depends on children’s age, developmental stage, the type of the ingested object, and clinical presentation. However, our study contends that the majority of FB ingestion can be moved spontaneously through stool by applying the noninvasive therapeutic approach without causing clinical complications.
Keywords
Foreign body ingestion
Children
Endoscopy
Guidelines
INTRODUCTION
The scenario of foreign body (FB) indigestion is considerably a significant problem in children because they are very keen to explore the environment by keeping the objects in their mouths. Unfortunately, a number of these tiny objectives can be unintentionally swallowed, and eventually, this has resulted in increasing parental anxiety.[1] The gender distribution of FB ingestion is relatively equal between boys and girls as well as a higher number of incidents is noted in the age ranging from 6 months to 3 years.[2] The majority of swallowed FBs are eliminated naturally through the gastrointestinal tract (GI) without causing any clinical complications although endoscopic and surgical approaches are required only in a few cases.[1,3] According to a recent research study, 80%–90% of particles were passed naturally through the GI tract without causing any complications while 10%–20% were removed by endoscopic procedures and there was only 1% required open surgery.[4] Because in some ingested phenomena, a foreign body cannot easily move through the part of the GI tract such as the pylorus, stomach, duodenum, and ileocecal valve.[2,5]
The common type of swallowed FBs is radiopaque including coins, screws, tiny magnets, safety pins, nails, plastic buttons, and button batteries though the radiolucent object like food particle impaction is to be considered in the ingested management.[4] The digestive tract FBs are frequently asymptomatic and ingestion likely mimics other conditions such as cough, vomiting, sore throat, and chest discomfort or abdominal pain.[6] The clinical diagnosis of FB ingestion in children is often challenging because children are unable to express the incidents and clinicians should not rely on it. However, the history of eyewitness accompanied adults may useful although usually more than 3 years of old children can give the history of ingestion themselves.[2] Most of the time FB ingestion is transiently discomfort and later becomes symptomless or can be presented with mild irritation, even rarely causing a life-threatening problem.[7] Some factors influence the necessity of emergency removal of FBs including the type, shape, size and site.[8] It is important to develop a comprehensive approach to the early recognition and timely management of ingested FBs.[2,9] Moreover, to reassure the anxiety of the parents and children, it is essential to have successful alleviation management to avoid developing complications regarding ingested cases.[10] The primary objective of this study is to assess the sociodemographic factors of ingested FB, its details as well as identify the efficient management of swallowed FBs and the key factors which influence the FBs removal procedure. As a result, this study will help to establish the guideline to manage the FBs ingestion in children and help to initiate the awareness programme in Sri Lanka.
MATERIAL AND METHODS
This study was conducted as a prospective analytical study in a tertiary care centre, in Sri Lanka for 1 year from 2019. This study aims to assess the particular aspects of FB ingestion including sociodemographic factors, and details of FB, and find the efficient clinical outcomes of a novel non-invasive interventional approach. Moreover, assessing the factors that influence the ingested FB removal in children, who were admitted to Lady Ridgeway Hospital, Sri Lanka. The novel non-invasive interventional approach combined with lactulose syrup, liquid paraffin syrup, domperidone syrup, and ducolax suppository according to the patient’s weight in addition to the victim was asked to the right lateral sleep. This study recruited 55 ingested children, who were documented as an index suspicion of FB swallowing while the exclusion criteria were aspiration of FB and were not given informed consent to participate in this study.
The data extraction form was used to collect sociodemographic, details of FB, clinical presentations, and therapeutic procedures from patients’ records, and additional information such as when, where, and who was accompanied with children were taken from the affected children and/or guardians. In this study, the setting was a tertiary care centre, the patients also were referred to this hospital’s emergency treatment unit from other community hospitals, where the endoscopy service was limited. Initially, all the patients underwent to a plain thoracic-abdominal radiological image within the 1st h of their admission regardless of the history of the incident and clinical symptoms. In some cases, the upper GI tract endoscopy was done by the same clinicians because some of the ingested FBs are radiolucent as receiving the negative X-ray of ingested materials. To achieve the study objectives initially, the descriptive analysis was carried out using the statistical software Statistical Package for the Social Sciences (version 26) to know the characteristics and distribution of variables and identifies the relationship between two variables. This descriptive analysis was conducted through two steps including univariate and bivariate analysis. The Chi-squared test was used to check the relationship between two categorical variables as this study dataset comprises more than 50 observations, where 5% is used as the significance level.
RESULTS
According to the histogram of age, children’s age ranged from 1 to 13 years whereas the mean age was 5.18 ± 3.1 years and the median was 5 years. Overall, ages were distributed as skewed to the right. Among this study participant, the gender ratio between boys and girls was 3:2 [Figure 1]. The majority of this study participant was from the Colombo district (47.3%) while the following common residential regions were Gampaha (27.7%) and Kalutura (14.6%). A larger number of swallowed children (n = 52) had appropriate developmental stages but only a few victims (n = 3) had a developmental delay. The higher number of ingested FB was metal (88.5%) although rubber, glass, and food particle accounted for only a small proportion 3.8%, 1.9%, and 1.9%, respectively. Among the larger number of metal FB ingestion, coins amounted to the highest proportion, at 33.3% while button battery was the second higher incident (29.4%). There were 13.7% and 5.8% recorded nail and jewellery items, respectively. It was noticeable that the largest proportion of shapes was round (62%) whereas both spherical and tubular were approximately one-tenth of round shape cases. However, there were 29% cases with irregular shape FBs ingestion. In addition, this study found that a larger proportion of swallowed FBs had no sharp edge as the ratio between sharp edge and non-sharp edge was 1:4. The greatest numbers of FBs were found in the stomach (70.7%) although the intestine was 17.1% and the upper and lower part of the oesophagus was 2.4% and 9.8%, respectively.

- Histogram of patients’ age.
This study identified that 62.9% of incidents occurred in the presence of adults despite the majority being passive (55.8%). This study found that the largest number of incidents (88.8%) happened at home while approximately 10% took place at pre-school and 7.4% occurred outside the home. Almost 98% of swallowed cases had been investigated through plain radiological images only 1.9% was undergone endoscopic examination. However, the majority of cases (90.3%) presented with asymptomatic of indigestive although very limited incidents (9.6%) were associated with clinical presentation of vomiting, sore throat, and cough. This study found that 88.8% of FB ingestions were passed spontaneously with a stool while 8.3% of cases required endoscopy removal but only 2.78% swallowed FBs eliminated naturally with vomiting [Figure 2]. However, none of the cases of this study had complications after the removal of FBs although greater numbers of cases (92.1%) were discharged within a day of admission to the hospital. In addition to that, it was noticed that a greater number of children both male (58.3%) and female (30.6%) were managed spontaneously to pass the FB with stool. All the cases treated with naturally vomiting (2.78%) were male; in comparison, all the endoscopy removal cases were female (5.56%). This study found that when the FB was located in the upper part of the oesophagus and intestine patients were only managed spontaneously with stool [Figure 3]. The following summarizes the factors with corresponding P-values, which show the statistically significant relationship with the procedure when the Chi-squared test was carried out [Table 1].
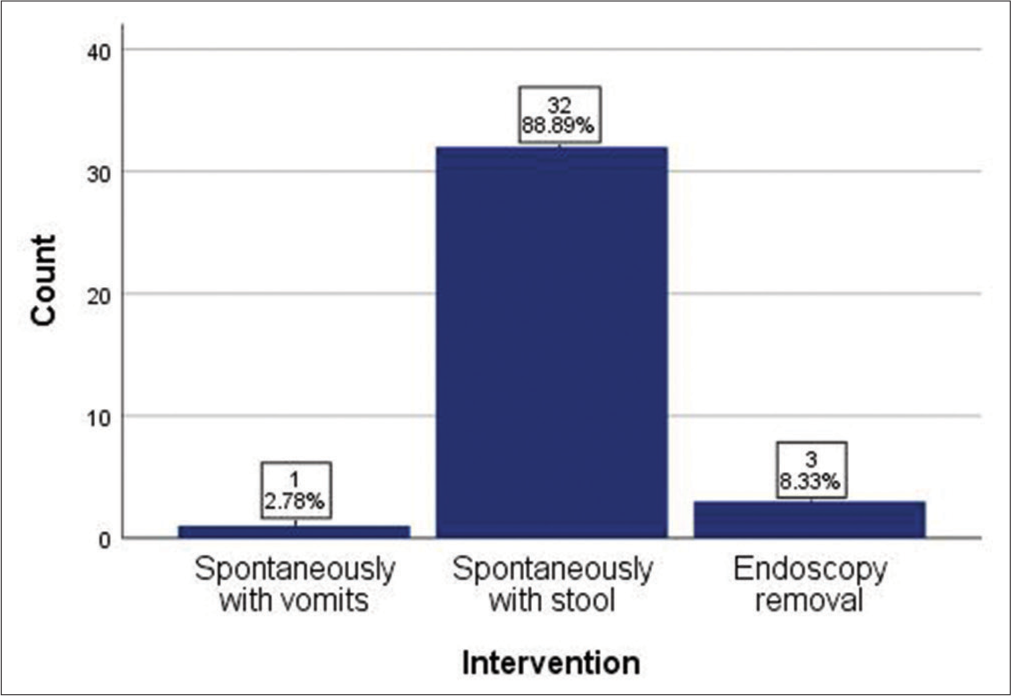
- Intervention approach of foreign body removal.

- Intervention approach and foreign body location in the gastrointestinal tract.
| Variables | P-value |
|---|---|
| Shape of FB | 0.000 |
| Sharpness of FB | 0.024 |
| Symptoms after incident | 0.000 |
| Investigation method | 0.003 |
DISCUSSION
The FB ingestion is a significant incident in paediatric clinical practice, most events occur in children ages ranging from 6 months to 3 years.[11] In our study, this showed that children’s age ranged from 1 to 13 years whereas the mean age was 5.18 ± 3.1 years and the median was 5 years. This study participant’s gender distribution between boys and girls was 3:2. These similar findings are consistent with other gender distribution reports related to FB ingestion a research study showed slightly male predominance.[3,4] It is largely acknowledged that the high prevalence of FB ingestion is identified in children because of their exploratory habits despite involving the gender difference between males and females.[12] The majority of this study’s participants were represented from the district where this study setting is located. This may help to come up with a postulation that FB ingested children were directly brought to the children’s specialty hospital rather than making delayed by admitting to other hospitals as the children accompanied by adults have a better awareness of the children’s care. However, this study found that 62.9% of incidents occurred in the presence of adults despite the majority being passive (55.8%).
A Romanian study claimed that in the clinical presentation consideration, common complaints were abdominal pain and vomiting 55.73% and 34.42%, respectively, also 29.5% of cases were asymptomatic ingested children.[1] However, in our study, the majority of cases (90.4%) presented with asymptomatic of indigestive FB with very limited incidents (9.6%) associated with clinical presentation of vomiting, sore throat, and cough. A similar result of a high prevalence of asymptomatic ingested incidents was reported in a number of other studies.[2,13] Our study suggests that the manifestations of indigested FB clinical features are depended on the type of FBs as a statistically significant relationship (P = 0.039) was found between types of FB and symptoms. In addition, factors such as sharpness of FB (P = 0.024), investigation method (P = 0.003), and symptoms after swallowing FB (P = 0.000) also showed a statistically significant relationship with the procedure, which was identified through the Chi-squared test. Moreover, our study included a wider range of ingested objects such as coins, button batteries, nails, jewellery, and unidentified objects though the most frequently swallowed FB was coins this similar finding was reported in another study (33.3%).[14] Furthermore, our study noticed that the ingestion of button batteries had the second higher (29.4%) incidence in children because this might be the age-specific preference as they frequently use toys in their early childhood stages.[13] However, in our study, all ingested button batteries were managed to pass spontaneously with stool despite considering a greater number of studies claim that button batteries should be removed immediately. Because of the high risk of sparking between the anode and cathode of the battery by the soft tissue of the GI tract, as well as, the high concentration of HCL in the stomach might cause degradation of the battery subsequently developing poison due to the chemical containing battery.
A retrospective study in a similar tertiary care clinical setting assessed the association between site and size of ingested FBs also investigated the relationship between the size and the clinical features. They stated that the expected results could not be objectified probably due to the heterogeneity of age distribution among the participated subjects.[15] In our study, participants had the similar heterogeneous distribution of age thus we could not objectify the association between the size of FBs and site as well as the clinical features. The plain radiological image is an essential diagnostic tool in swallowed FB cases in the main initial investigation approach.[16] In our study, almost 98% of swallowed cases had been investigated through plain radiological images only 1.9% had been examined by endoscopy although a number of studies reported X-ray identification that ranged from 63.1% to 96.4%.[17,18] Our study tends to agree with other authors who claimed that the optimal clinical procedure for removing the FB is largely dependent on many factors including the children’s age, the clinical features, type, shape, location, and sharpness of the FB.[19] The drawn clustered bar chart between interventional procedure and shape of FB indicates that a high percentage of children treated spontaneously with the stool were swallowed round shape of FB (64.7%) while it was only 5.9% spherical shape of FB and there were no cases in a tubular shape. Moreover, a statistically significant relationship between procedure and shape of FB was identified (P = 0.000) through the Chi-squared test. When considering the age factor, the average age of endoscopy removal was 7.7 years compared to the average age of patients in other procedure methods such as spontaneously with stool (5 years) and spontaneously with vomiting (3 years). Furthermore, all the cases treated with endoscopy removal (8.3%) consisted of only normal developmental stage and all were metal FBs. Furthermore, it was found that most of the asymptomatic patients (88.9%) were managed spontaneously with stool and among the symptomatic patients (9.6%) only 5.6% were managed by endoscopy removal. Therefore, endoscopy removal could be suggested for the normal developmental stage of children at approximately 7 years of age and incidents of metal FB ingestion with asymptomatic cases. Furthermore, an endoscopy therapeutic method is quite expensive and it requires general anaesthesia before the procedure but this procedure is more challenging and potential risk for the younger population. Considering the study limitations, this study participant’s age had a wider range of 1–13 years as a result of the heterogeneous distribution of age, we could not objectify the association between the size of FBs and location additionally, a similar problem has been encountered for assessing the relationship between FBs and clinical features of FB ingestion. Moreover, in our study, the majority of ingestion FB type was metal; however, other type of FBs was very limited thus we are unable to evaluate the association between other types of FB with our therapeutic procedure.
CONCLUSION
FB ingestion is a potentially serious problem that peaks at a younger age. There are a number of studies that claim that the management of this pathology relatively depends on the patient’s age, developmental stage of children, the type of the ingested objects, and the clinical presentations. However, our study findings contend that the majority of ingested FBs can be passed spontaneously through stool by applying the non-invasive therapeutic approach without causing clinical complications despite considering other factors such as age, gender, and type of FBs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Foreign body ingestion in pediatrics: Distribution, management and complications. Medicina. 2019;55:686.
- [CrossRef] [PubMed] [Google Scholar]
- Inpatient pediatric foreign body ingestion: National estimates and resource utilization. J Pediatr Gastroenterol Nutr. 2021;73:37-41.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign bodies ingestion in children: Experience of 61 cases in a pediatric gastroenterology unit from Romania. Gastroenterol Res Pract. 2016;2016:1982567.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic retrieval of two intragastric spoons at least seven years after ingestion. Laparosc Endosc Rob Surg. 2019;2:77-9.
- [CrossRef] [Google Scholar]
- Endoscopic management of foreign bodies in the gastrointestinal tract: A review of the literature. Gastroenterol Res Pract. 2016;2016:8520767.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign body ingestion in children. Clin Endosc. 2018;51:129-36.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with removal of impactted fishbone in children, suspected ingestion. Pediatr Gastroenterol Hepatol Nutr. 2016;19:168.
- [CrossRef] [PubMed] [Google Scholar]
- Management of ingested foreign bodies in children. J Pediatr Gastroenterol Nutr. 2015;60:562-74.
- [CrossRef] [PubMed] [Google Scholar]
- Quality improvement in pediatric endoscopy: A clinical report from the NASPGHAN endoscopy committee. J Pediatr Gastroenterol Nutr. 2017;65:125-31.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic management of foreign bodies in the upper gastrointestinal tract: A review. World J Gastrointest Endosc. 2014;6:475.
- [CrossRef] [PubMed] [Google Scholar]
- The value of ultrasound in the investigation of ingested foreign bodies in children. Sonography. 2018;5:51-60.
- [CrossRef] [Google Scholar]
- Foreign body ingestion in children. Türk Pediatri Arsivi. 2015;50:234-40.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent abdominal pain in children: A clinical approach. Singapore Med J. 2015;56:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Paediatric gastrointestinal endoscopy: European society for paediatric gastroenterology hepatology and nutrition and european society of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr. 2017;64:133-53.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of radiopaque gastrointestinal foreign bodies expelled by spontaneous passage in children: A 15-year single-center study. Front Pediatr. 2018;6:172.
- [CrossRef] [PubMed] [Google Scholar]
- Review of ingested and aspirated foreign bodies in children and their clinical significance for radiologists. Radiographics. 2015;35:1528-38.
- [CrossRef] [PubMed] [Google Scholar]
- X-ray detection of ingested non-metallic foreign bodies. World J Clin Pediatr. 2014;3:14.
- [CrossRef] [PubMed] [Google Scholar]
- Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019;14:26.
- [CrossRef] [PubMed] [Google Scholar]
- Management of foreign body ingestion in children with cerebral palsy: Need for proper trauma management protocol. J Fam Med Prim Care. 2018;7:638.
- [CrossRef] [PubMed] [Google Scholar]






