Translate this page into:
Coronavirus disease 2019 associated stroke in a toddler – A case report
*Corresponding author: Neeraj Gupta, Department of Paediatrics, Sir Ganga Ram Hospital, New Delhi, India. drneeraj1979@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sawhney N, Mendiratta L, Gupta N. Coronavirus disease 2019 associated stroke in a toddler – A case report. Karnataka Paediatr J 2021;36:132-4.
Abstract
Background:
Stroke, an infrequent entity in children, usually presents with headache, reduced cognition, and seizures as frequent findings. The association of paediatric stroke with Coronavirus disease 2019 (COVID-19) is unknown with only a hand full of postulated hypotheses till date.
Clinical Description:
A 2-year-old child with sudden onset focal neurological deficits and high COVID antibody titters has been reported soon after a brief episode of cough and cold. Magnetic resonance imaging brain suggested infarct in posterior cerebral circulation. All other inflammatory markers and prothrombotic work-up were normal pointing toward a territorial affliction.
Management:
Child responded well to anticoagulants (low molecular weight heparin and aspirin) with complete neurological recovery.
Conclusion:
Possibility of COVID-19 associated regional endotheliitis is very high in the aforesaid toddler. Our case is the youngest reported case of paediatric stroke with a possible association with COVID-19.
Keywords
Coronavirus disease 2019
Stroke
Toddler
Endotheliitis
Endotheliopathy
INTRODUCTION
The ongoing Coronavirus pandemic has affected nearly 100 million people globally till February 10, 2021.[1] The paediatric population at large is asymptomatic or present with mild upper respiratory and gastrointestinal symptoms only.[2] Neurological manifestations in coronavirus disease 2019 (COVID-19) can vary from involvement of the central nervous system in form of seizures, encephalopathy, large vessel stroke, and acute necrotizing encephalitis; peripheral nervous system with Guillain-Barre syndrome such as features and skeletal muscles, as well as early alterations of olfaction and taste.[3] In contrast to adults children show fewer neurological complications.[4]
CLINICAL DESCRIPTION
A previously healthy 2-year-old boy had mild cough and cold 3 days before presentation. On the next day, parents noticed increased irritability in his behaviour. He was brought to the hospital as he developed outward deviation of the left eye with abnormal gait on the 3rd day of illness. There was no history of recent onset of fever, shortness of breath, skin rashes, vomiting, seizures, trauma, or vaccination. There was a history of mild fever and cough for short duration in father 2 weeks back, who did not require any medical intervention. At admission, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA was not detected in nasopharyngeal swab. On examination, the child was irritable with left 3rd cranial nerve palsy and ipsilateral mild hemiparesis. Fundus examination was within normal limits. Magnetic resonance imaging brain and neck with angiography depicted restricted diffusion in posterior cerebral circulation suggestive of infarct with no apparent thrombus or emboli [Figure 1a and b]. 2D-Echocardiography did not reveal any thrombus or coronary artery dilatation. Pro-thrombotic investigations including lipoprotein A (19.8 mg/dL), homocysteine levels (6.85 μmol/L), Factor V (110%), Vitamin B12 (193 pg/mL), haemoglobin (10.2 g/dL), normocytic normochromic picture on peripheral smear, iron 21.3 μmol/L, platelet count (4,23,000/μL), APTT (30.8 sec), INR (0.97), antithrombin activity (124%), fibrinogen (2 g/L), protein C (90.7%), and S (73.6%) activities were within normal limits. Investigations such as antinuclear antibodies, perinuclear anti-neutrophil cytoplasmic antibodies, cytoplasmic anti-neutrophil cytoplasmic antibodies, antiphospholipid antibodies, anti-proteinase 3, and myeloperoxidase for vasculitis and other rheumatological causes were unyielding. His serum COVID antibodies were high (total 234 s/c and Immunoglobulin G 18.7 s/c), which were determined by VITROS Immunodiagnostic Products anti-SARS-CoV-2 total assay, manufactured by Ortho Clinical Diagnostics. Inflammatory markers such as ferritin (10 ng/mL), interleukin-6 (1.27 pg/ mL), lactate dehydrogenase (348 IU/L), C-reactive protein (negative), and NT-proBNP (31 pg/mL) were within normal limits.
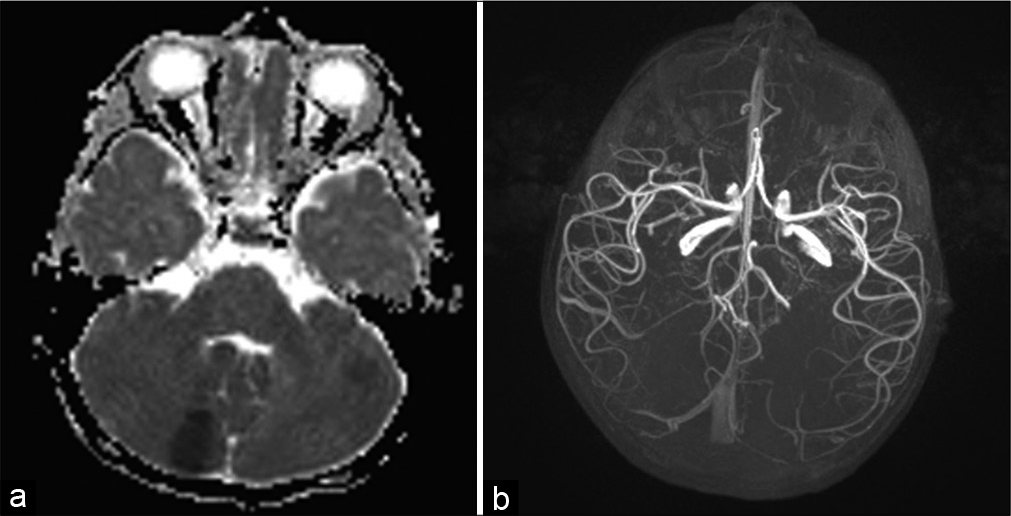
- (a) Focal areas of restricted diffusion in midbrain and left cerebellum. (b) Normal arterial circulation.
MANAGEMENT AND OUTCOME
The child was started on oral aspirin (5 mg/kg/day) and low molecular weight heparin (20 units/day) subcutaneously. During the hospital stay, his irritability reduced without further progression of neurological status. He was discharged home, after 4 days of stay, on oral aspirin and rehabilitation advise. During follow-up, neurological weakness improved over next 3–4 weeks and oral aspirin was stopped after a total of 8 weeks duration. No new symptom appeared during the follow-up.
DISCUSSION
Paediatric stroke is an uncommon event with an annual incidence of 1.3–1.72 cases per 100,000 children <18 years of age.[5] Due to the non-specific and subtle nature of symptoms most cases are frequently under-diagnosed. Acute ischemic stroke attributes to more than half of the cases most often presenting as focal neurological defect followed by headache, altered sensorium, and seizures.[6] Our patient presented with features of cranial nerve palsy, hemiparesis, and non-specific behavioural abnormality. Common causes such as cardiac, haematological including prothrombotic states, post-infectious (influenza, HIV, hepatitis B/C, varicella, herpes simplex, and Mycoplasma), and arteriovenous malformations, metabolic states including hyper-homocystenemia, vasculitis, drugs, and trauma were ruled out. High COVID antibody titer and history of recent contact with a viral episode in father raised the possibility of COVID-19 associated neurological phenomenon in the child.
Only few cases of COVID-19 associated paediatric stroke have been reported till date.[6] The odds of stroke is 7.6 folds higher with COVID-19 when compared to influenza.[7] School age children have been the youngest reported cohort associated with features of systemic inflammation.[6] Hypercoagulable state, vasculitis, and cardiomyopathy are the predominant mechanisms described for COVID-19 associated ischemic strokes.[8] Angiotensin Converting Enzyme-2 receptors, being the entry point for SARS CoV-2, are present in endothelial and arterial smooth cells in brain, lungs, heart, small bowel, and kidneys.[9] Direct invasion of endothelial cells is responsible for endotheliopathy, which can trigger thrombotic and inflammatory cascades through complement system activation.[10] Viral inclusions in endothelial cells are also responsible for endothelial dysfunction and apoptosis.[11] Endothelial dysfunction, in turn, causes vasoconstriction, organ ischemia, tissue edema, and further worsening of procoagulant state.[12,13] Cytokine storm with hypercoagulable state can also be associated with post COVID multisystem inflammatory syndrome in children (MIS-C).[11] Although our patient had neurological complications with high antibody titters, yet he did not complete the criteria for MIS-C as the inflammatory markers were normal and no other system was involved.[14]
Possible pathophysiological mechanism in the index patient could be either para-infectious or immune mediated regional endotheliitis. Tissue biopsy might be of help for definite diagnosis but the feasibility and risk of intervention needs to be carefully balanced. Crippa et al. have found endotheliitis as probable cause of stroke in a 24-year young man associated with mild COVID-19.[15] As per the literature search, our patient is the youngest case to be reported till date who was affected with COVID-19 associated stroke, without any sign of systemic inflammation, with endotheliitis as probable etiology.
With the ongoing pandemic and associated increase in the number of stroke cases in paediatric population, clinicians must keep COVID-19 infection and following immune response as one of the highly suspicious causes. Large multicentre trials are needed to confirm this association. Till then an unbiased strategy should be followed to find the etiology and aggressive management should be done to avoid any neurological sequelae.
KEY MESSAGES
Hypercoagulable states, vasculitis, and cardiomyopathy are known mechanisms for COVID-19 related stroke
Para-infectious or immune mediated endotheliopathy is the probable etiology in the index patient
Youngest stroke case reported with possible COVID-19 association.
CONCLUSION
A high index of suspicion for COVID-19 associated phenomenon is warranted in children presenting with clinical findings, which are otherwise unexplained during routine work-up, especially in the current pandemic era.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of Interest
References
- Coronavirus Disease (COVID-19) Outbreak Situation. 2021. Geneva: World Health Organization; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Last accessed on 2021 Feb 10]
- [Google Scholar]
- SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663-5.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological manifestations of COVID-19: A brief review. Indian J Med Res. 2020;152:41-7.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19: Neurological considerations in neonates and children. Children (Basel). 2020;7:133.
- [CrossRef] [PubMed] [Google Scholar]
- Focal cerebral arteriopathy in a COVID-19 paediatric patient. Radiology. 2020;297:E274-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arteritis and large vessel occlusive strokes in children following COVID-19 infection. Paediatrics. 2021;147:e2020023440.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020;77:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological complications of coronavirus and COVID-19. Rev Neurol. 2020;70:311-22.
- [CrossRef] [PubMed] [Google Scholar]
- Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of stroke in COVID-19. Cerebrovasc Dis. 2020;49:451-8.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial dysfunction a marker of atherosclerotic risk. Arterioscl Throm Vas. 2003;23:168-75.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417-8.
- [CrossRef] [Google Scholar]
- COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020;20:e276-88.
- [CrossRef] [Google Scholar]
- Stroke in a young adult with mild COVID-19 suggesting endotheliitis. New Microbes New Infect. 2020;38:100781.
- [CrossRef] [PubMed] [Google Scholar]






