Translate this page into:
Diagnostic value of flexible fibre optic bronchoscopy in the evaluation of children with suspected airway foreign body: A retrospective study
*Corresponding author: Abhijit Venkatesh Joshi, Department of Pediatrics, Chiranjeev Children’s Hospital and Critical Care Center, c/o Chiranjeev Children’s Hospital, Aurangabad, Maharashtra, India. joshiabhijit71@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Khandelwal SM, Khadke RR, Joshi AV. Diagnostic value of flexible fibre optic bronchoscopy in the evaluation of children with suspected airway foreign body: A retrospective study. Karnataka Paediatr J. 2024;39:145-9. doi: 10.25259/KPJ_30_2024
Abstract
Objectives:
To evaluate the role of flexible fibre optic bronchoscopy in the diagnosis of suspected airway foreign bodies in children.
Material and Methods:
A retrospective study of suspected airway foreign bodies in 124 cases in children was done.
Results:
Results were obtained in terms of percentage of cases in which foreign body was seen, age incidence, sex difference, type of foreign body, history, bronchoscopy findings and findings of other relevant radiological investigations and data compiled and compared with some other retrospective studies
Conclusion:
The negative predictive value of a diagnostic bronchoscopy in viewing a foreign body is high and can also guide in finding other causes for the obstruction. It also provides an opportunity for other procedures, such as tracheo-bronchial lavage and suctioning of secretions, in addition to removal of foreign bodies in some.
Keywords
Bronchoscopy
Fibre optic
Children
Aspiration
INTRODUCTION
Paediatric foreign body (FB) aspiration is one of the potentially serious and common household problems of significance presenting to the emergency room. Children of a younger age are vulnerable to foreign body aspiration.
This is attributed to children’s curiosity and tendency to explore the environment in this particular age group. Furthermore, children with developmental and psychological disorders are more prone to have foreign body aspirations. A higher incidence is seen in children with congenital malformations, as mentioned in some previous studies [Pie chart 1].[1]
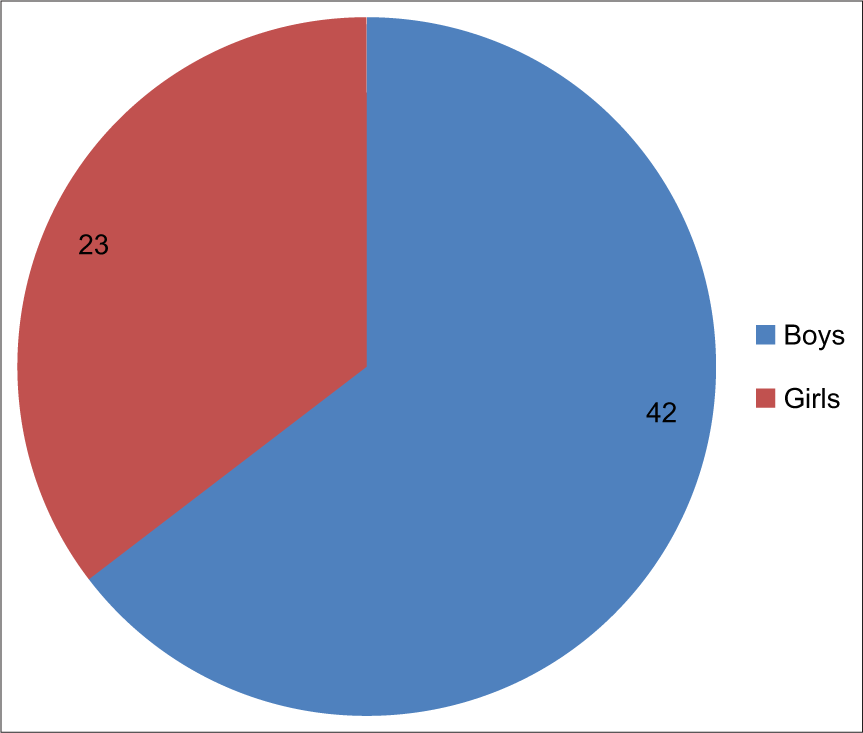
- Sex difference in foreign body (FB) aspiration in total 65 cases.
The incidence of FB aspiration is higher in boys than girls and this sex predilection may be related to different physical and psychomotor development seen in both sexes and also to the methods of parenting and sex ratio of the population.[2]
With a confirmed history of choking followed by repeated coughing episodes, the possibility of a foreign-body aspiration should be sought.
The various settings related to a foreign body aspiration in a child need to be considered:
As compared to children of other ages, children <1 year old are immediately attended to in case of emergency as they are less developed verbally. Children more than 6 years of age can clearly express concern and show discomfort in aspirated foreign bodies.
The location of an FB, when it is trapped beyond the trachea, is seen mainly in the right bronchus owing to a larger angle between the right main bronchus and the airway.
The FB type, whether organic or non-organic, depends many times on the dietary habits of the region involved.
Airway FB is often missed clinically or radiologically initially but comes with complications that arise due to an old retained FB. They may cause complications such as obstructive emphysema, atelectasis, and co-morbid long-term pulmonary infection or sometimes even bronchopneumonia. Other lesser-known complications are pulmonary bulla, pleural effusion and pneumothorax with mediastinal emphysema.[3]
The delay in the diagnosis of airway FB in children has many reasons.
As per the literature, only 16–40% of cases show a classic triad of sudden-onset choking, coughing and wheezing or unilaterally decreased air entry.[4]
Various paediatric common illnesses such as bronchiolitis, pneumonia or asthma can be confused with a similar presentation.
Lower airway foreign bodies can present with subtle or non-specific symptoms of lower respiratory tract involvement. Complications arising from non-indicated treatment such as steroids, antibiotics and bronchodilators further add to the confusion. The differentiation from many chronic childhood illnesses such as pulmonary infections, bronchiectasis, asthma and lung collapse or lung abscess can become difficult.
The chest X-ray has a poor diagnostic yield in the diagnosis of airway FB. It can detect only 16% of radio-opaque foreign bodies. A negative X-ray alone however does not exclude a foreign body diagnosis.[1] It is even difficult to pick up complications arising from a retained FB like emphysema or atelectasis. As a comparison, chest computed tomography (CT) has a high sensitivity (99%) and specificity (92%) for the detection of airway FB, but a negative CT scan, at the same time, does not necessarily rule out an FB.[5]
With a high clinical suspicion, irrespective of whether the history is suggestive of FB ingestion or not, both rigid and flexible bronchoscopy is implicated in FB removal in children. The role of rigid bronchoscopy remains unequivocal in diagnosing and removing only established airway FB confirmed either on history or by clinical examination or radiologically. In cases with high clinical suspicion or a history indicative of aspiration, in radio-lucent objects, the role of flexible bronchoscopy is noteworthy. It can also be considered in the removal of certain paediatric cases in expert hands.
MATERIAL AND METHODS
The record of patients who had undergone flexible fibre optic bronchoscopy for foreign body evaluation in Varad Children’s Hospital, Aurangabad, India, from 2017 to 2022 was retrospectively evaluated.
A retrospective study of 124 cases was conducted in which a paediatric airway foreign body was suspected and flexible fibre optic bronchoscopy was done. The parameters considered were the age group, sex of the child, clinical presentation, other supportive radiological investigations, and their results, outcome of fibre optic bronchoscopy, types of FB visualized, and complications.
The points under consideration were:
-
Initial clinical presentation:
The cases were grouped taking into view the clinical presentation; some presented with a history of choking and some with a strong clinical suspicion on the part of the referring physician. In some cases, a non-resolving pneumonia was present or recurrent respiratory involvement was seen at a particular location. In some, either a chest X-ray or a CT scan guided this.
-
Investigations done before the fibre optic bronchoscopy:
An X-ray chest was ordered in all cases in which FB was suspected. The various findings detected on an X-ray consisted of lung hyperinflation, either unilateral or bilateral, collapse of a part or a lobe , and pneumothorax. They are depicted in Graph 1.
 Graph 1:
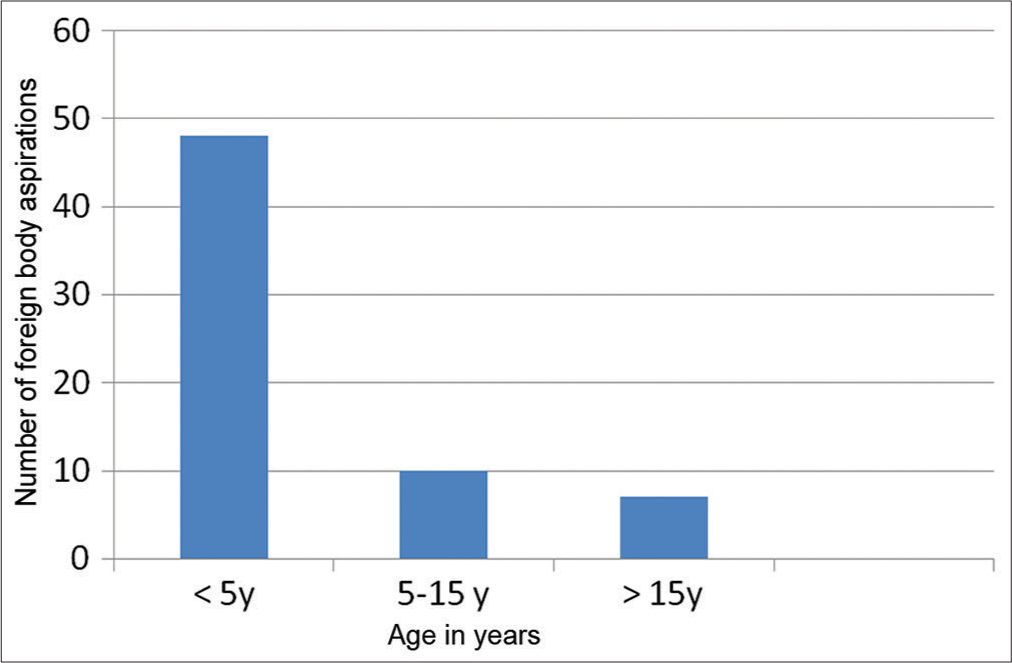
Graph 1:- Age-specific foreign body (FB) aspiration incidence in 65 cases.
-
Procedure:
The diagnostic bronchoscopy was done with a 3.5 mm fibre optic Pentax flexible bronchoscope with a working channel of 1.2 mm. The bronchoscope is supported with a side port which can be utilized either for flushing the lumen during bronchoscopy as well as for instillation of a local anesthetic. The exact duration of time required from start to the end was also noted. A mild sedation was achieved with a short-acting benzodiazepine like midazolam, and a 2% xylocaine solution was instilled at the level of vocal cords or trachea after the bronchoscope was introduced. Complications, if any, were noted.
The findings of the procedure were noted and are presented in the results section.
The findings are presented in a tabular form and analysed [Table 1].
| FB detected | 65 (124) |
| History | |
| History of choking | 27 (21) |
| History of cough | 45 (37) |
| Wheezing | 18 (15) |
| X-ray findings | |
| Normal | 31 (47) |
| Hyperinflation | 21 (32) |
| Right side | 10 |
| Bilateral | 4 |
| Left | 6 |
| Lung collapse | 10 (15) |
| Right side | 6 |
| Left side | 4 |
| Pneumothorax | 3 |
| Type of FB | |
| Organic | 52 (80.25) |
| Inorganic | 13 (19) |
FB: Foreign body.
RESULTS
A foreign body could be visualized in 65 of the total 124 cases. The remaining cases were grouped as:
42 cases consisted of a normal tracheo-bronchial tree.
12 cases were seen to have copious secretions and mucus plugs, which were suctioned but no FB was found.
5 cases were suspected to have an extrinsic compression visualized from inside the lumen and were referred back to the treating physicians to get further relevant investigations done but the track of the records was not kept for this study.
The fibre optic bronchoscopy was found very useful in detecting the site, location and type of FB. It helped to check for partial or complete airway obstruction. A search was also made to look for any granulation tissue surrounding it or take out the secretions during the procedure.
The FBs were again divided into organic and non-organic. The organic FB mostly comprised of peanuts, cashew nut pieces, almond pieces, coconut fragments, turmeric and chikoo seeds and small food particles in some. The non-organic FBs were mostly small plastic beads and pebbles. The findings are also presented in a tabular form [Table 1].
In our study of 124 cases in which fibre optic bronchoscopy was performed, no complications were observed.
DISCUSSION
In our experience, the information gained from fibre optic bronchoscopy could be utilized for rigid bronchoscopy in FB removal with safety according to the site, type, nature of the FB and its associated complications detected on fibre optic bronchoscopy.
The location of the aspirated FB depends upon the age of the child and the position/posture at the time of aspiration. In the majority of cases in our study, the FB was removed from the right main bronchus as compared to the left, which explains the wider and steeper anatomy of the right main bronchus; but in infants and smaller children, due to the predominance of left main bronchus, the aspiration was also seen on the left in younger age group.
Complications like obstructive emphysema, atelectasis, or co-morbid associated complications like bronchopneumonia were seen rarely in our study. This shows the relatively lesser incidence of a retained FB in our study, in which more inflammation and infection are expected.
The aspiration of organic versus non-organic FB was studied only to show a relatively higher incidence of organic FB in our study. Peanut piece was a common object obtained reflecting society and family’s social, cultural and dietary habits.[6]
This probably is attributed to the low cost and availability of peanuts in our region.
Choking and coughing, which are the likely events to be associated with FB aspiration, had an account only in a small percentage of children. This could be due to a lower age at presentation, having lesser verbal cues from the patients in the event of aspiration and the failure of the parents to recognize the symptoms early. Other cases with a high incidence were referrals from physicians in the setting of persistent respiratory symptoms.
The children were subjected to chest radiography in all cases. Among many normal X-ray findings when FB was recovered later, the most noticeable radiological findings were obstructive emphysema, localized or generalized, atelectasis or a partial lobe collapse. Longer retention time of FB, particularly an organic type, can give rise to complications of pneumonia and collapse consolidation.[7]
The diagnostic fibre optic bronchoscopy lasted for an average duration of 2–3 min and was relatively a shorter time compared to some other studies. The longer time required in other case studies might be attributed to the FB removal in the same setting which was possible due to the availability of expertise[7] and a rigid bronchoscope apparatus. In our study, only a diagnostic study was conducted, taking less time. The advantage of this study lies in the very short exposure to mild sedation and local anaesthesia which subjected the children to very low risk.
The only limitations of this study are seen as follows: This was an experience from a single centre and cannot be uniformly applied to all. CT scan of the chest which has a comparable sensitivity and specificity was not available for many of the children in our study.
No other diagnostic modality could give the information we achieved with a diagnostic fibre optic bronchoscopy and was superior to a more invasive rigid bronchoscopy,[8] the advantages also being a wide margin of safety and doing so with relative ease.
CONCLUSION
The yield of a clinical examination in the confirmation of a suspected airway foreign body is low. This is attributed to the low sensitivity and specificity of a good clinical examination in the identification of a penetration syndrome merely on the auscultatory findings.
A good radiological examination in the form of an X-ray may also have a poor interpretation and is based on variables like inspiratory or expiratory films and their reporting.
Doing a CT chest might add to the information gained from history clinical examination and equivocal X-ray interpretation, but it is sometimes not available or not feasible in some situations.
Fibre optic bronchoscopy can be implicated in the confirmation of airway FB and to gain information about the location, the nature, the type of obstruction, impacted or partially impacted and its mobility, the amount of granulation tissue present and other inflammatory signs seen and can be done safely in expert hands with a minimum of anaesthesia required. It helps in the proper visualization of the airway with its smooth passage to visualize the distal airways with precision. It helps in suctioning the secretions which can be analysed for cytology and bacteriological studies. As mentioned in the literature, this can even be the method of removal of some of the foreign bodies in expert hands.
Various disadvantages of a rigid bronchoscope to consider are as follows:
Bronchi, upper or subsegmental, are not readily visible with a rigid one
There are limitations to using a rigid bronchoscope for patients with cervical spine, mandible or head abnormalities
Not suitable for FB in peripheral airways, especially those in the upper lungs
Highly operator-based and qualified personnel are limited
Complications associated with rigid bronchoscopy are hypoxemia, tracheal bronchial lacerations or bleeding, laryngeal oedema, broncho-laryngospasm, pneumothorax, pneumomediastinum, re-intubation, mechanical ventilation, cardiac arrest, anoxic brain injury, etc.
More invasive and risky procedures of rigid bronchoscopy can be spared only for a confirmed FB and after getting its relevant details from a diagnostic modality like fibre optic bronchoscopy.
Ethical approval
Institutional review board approval is not required as this is a retrospective study in children for diagnostic purposes only.
Declaration of patient consent
Informed consent was taken before bronchoscopy was done in all cases. Declaration of patient consent for this study was not required as patients’ identity was not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Airway foreign bodies: A critical review for a common pediatric emergency. World J Emerg Med. 2016;7:5-12.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics and treatment of pediatric tracheobronchial foreign bodies: A retrospective analysis of 715 cases. Med Sci Monit. 2022;28:e937928-1.
- [CrossRef] [Google Scholar]
- Foreign bodies in pediatric otorhinolaryngology: A review. Pediatr Rep. 2024;16:504-18.
- [CrossRef] [PubMed] [Google Scholar]
- Nonfatal choking-related episodes among children-United States 2001. MMWR Morb Mortal Wkly Rep. 2002;51:945-8.
- [Google Scholar]
- Diagnostic value of various investigations in children with suspected foreign body aspiration: Review. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:248-52.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical analysis of bronchoscope diagnosis and treatment for airway foreign body removal in pediatric patients. Italian J Pediatr. 2022;48:159.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign body aspiration In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531480 [Last accessed 2023 Jul 31]
- [Google Scholar]
- Rigid bronchoscopy in foreign body aspiration diagnosis and treatment in children. Children (Basel). 2021;8:1206.
- [CrossRef] [PubMed] [Google Scholar]






