Translate this page into:
Efficacy of the Ponseti method in the treatment of neglected idiopathic talipes equinovarus at a tertiary hospital in Nigeria
*Corresponding author: Joseph Asuquo, Department of Orthopaedics and Traumatology, University of Calabar, Calabar, Nigeria. itansuq@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Anetekhai WI, Lasebikan OA, Asuquo J, Anetekhai CJ, Asuquo BJ. Efficacy of the Ponseti method in the treatment of neglected idiopathic talipes equinovarus at a tertiary hospital in Nigeria. Karnataka Paediatr J. 2024;39:14-9. doi: 10.25259/KPJ_1_2024
Abstract
Objectives:
Neglected clubfoot is common in our environment, for multifactorial reasons. It could cause pain and psychological distress to the patient and parents. We assessed the efficacy of the Ponseti method in the treatment of neglected clubfoot in a Nigerian Hospital.
Material and Methods:
This was a 15-month prospective and interventional study. Patients at least one-year-old with untreated idiopathic talipes equino varus (ITEV) or inadequately nonoperatively treated ITEV were the study population. The number of castings required for correction, tenotomy rate, dorsiflexion angle before and after tenotomy, and abduction angle after treatment were obtained. The chi-square test of independence was used to test the relationship between categorical variables. Logistic regression was used to assess if the Pirani score at the presentation predicted a successful correction at the end of the study. The level of significance was set at P < 0.05.
Results:
Forty-two children with 69 club feet were treated in this study. The mean age of presentation was 27.45 months (standard deviation [SD] = 19.22). The mean number of casting sessions required to achieve correction was 6.35 (SD = 1.95). The mean Pirani score at presentation was 4.27 (SD = 1.33) which reduced to 0.30 (SD = 0.35) after correction. The Pirani score at presentation had a positive correlation with the number of casts required for correction (r = 0.505, P < 0.001) but did not predict a successful correction after treatment. The success rate was 85.5%.
Conclusion:
The Ponseti method of treatment showed a high success rate in the treatment of neglected ITEV.
Keywords
Neglected clubfoot
Ponseti technique
Efficacy
Tenotomy
INTRODUCTION
Congenital talipes equinovarus (CTEV), or idiopathic talipes equinovarus ‘aka’ clubfoot, is the most common complex developmental foot and ankle deformity in children.[1] Children with CTEV commonly present at birth or shortly after that, as all newborns are screened for this deformity by the midwife, and any suspicions are reported appropriately for early review and management in developed nations.
A neglected CTEV is thus defined as one that has not been treated before walking age or which has had an inadequate or inappropriate initial treatment (that is, a treatment that has never resulted in correction, distinguishing it from cases of relapse) with deformity present at the time of walking.[2,3] African children are known to develop gross motor skills early compared to their Caucasian counterparts. Iloeje et al., in a study done in Southeast Nigeria, showed that children walk well alone at the age of 9–12 months, depending on the sex, as females walked earlier.[4] For this study, the walking age was set at 12 months. However, neglect is a problem in developing nations where ignorance, social stigma, poverty, and a lack of proper healthcare infrastructure militate against early presentation and treatment of children with CTEV.[2,5] These children often have pain, disability, callosities, rigidity, corns, ulcers, atrophy of the affected limb, and a poor psyche, especially in the much older ones who suffer from discrimination.[2,6]
The objective of the various treatment modalities that have evolved over time is to achieve a painless, supple, and plantigrade foot with good mobility without the need for orthoses. Treatment strategies that have been applied include extensive soft-tissue releases, external fixation, corrective osteotomies, triple arthrodesis, serial manipulation, and casting. Extensive surgical procedures are fraught with problems, including being of longer duration, resulting in a persistently painful and stiff foot in about half the cases on long-term follow-up and incomplete correction. The Ponseti method of serial manipulation and casting is preferable to the aforementioned treatment strategies, which produce morbidities that are almost always present in adulthood. Ponseti summarises it as follows: ‘The successful non-operatively treated foot is much better than the successful surgically treated foot.’ The Ponseti method of treatment has evolved to be the gold standard for the treatment of clubfoot in the past two decades.[1,2,7]
The literature abounds with studies on children who presented early, as Ponseti himself treated children six months and less with a successful correction in 90% of cases. The aim was to determine the success rate of the Ponseti method in the treatment of neglected CTEV and to relate the Pirani score(s) of the feet at presentation to the efficacy of the Ponseti method of treatment.
MATERIAL AND METHODS
The study was conducted at a regional tertiary Nigerian hospital located in the Southeast of Nigeria. Children attending the Clubfoot clinic of the hospital who met the inclusion criteria were recruited following documented informed consent. They were enrolled in the study after detailed consultation with their parents and/or guardians, highlighting the benefits and potential risks of the study and that prejudice shall not be given to their treatment should they decline consent at any time, even when previously enrolled. Fifteen-month prospective and interventional study (from June 1, 2018, to September 30, 2019) with recruitment of consecutive patients that fulfilled the inclusion criteria was adopted. The first 12 months were for recruitment and treatment, while the last three months were only for treatment of the children recruited on the 12th month of the study. The treatment lasted a maximum of 3 months. The efficacy of treatment was assessed at the removal of the last cast during the treatment period.
Forty-seven patients were recruited for the study. Five patients did not complete the treatment protocol as they were lost to follow-up at the time of the study. A total of 42 patients with 69 neglected feet completed the study.
Inclusion criteria
Children 1 year and above with untreated idiopathic CTEV and inadequately nonoperatively treated idiopathic CTEV patients a year and older with a minimum Pirani score of 1 were included in the study.
Exclusion criteria
Syndromic CTEV, secondary talipesequinovarus, for example, poliomyelitis, cerebral palsy, post burns, previous surgical intervention, those older than 16 years with idiopathic CTEV, and those that declined consent were excluded from the study.
A researcher designed pro forma was used to obtain patients’ details. A goniometer (Plastic universal standard goniometer) was used to measure passive foot dorsiflexion and abduction angles.
The following parameters were documented during the study:
Outcome variables
Independent variables
Age at presentation, sex, and laterality (unilateral or bilateral)
Pirani score before the commencement of treatment
Number of manipulations and casting required for correction
Need for tenotomy
Degree of passive ankle dorsiflexion before and after treatment
Passive abduction angle at the end of casting.
Dependent variables (outcome measures)
Any patient who did not meet the following criterion was considered to have failed treatment; post-treatment Pirani score of 0 or 0.5, with or without percutaneous tendoachilles tenotomy and/or anterior tibialis tendon transfer at the end of 3 months of treatment.
The success rate is defined below:
The procedure was the standard Ponseti method of manipulation and casting in an outpatient setting.
An abduction angle of 30–60° was the goal; this was due to the relative difficulty in manipulating older children.
Percutaneous tendoachilles tenotomy was done if, at full correction of the cavus, adducts, and varus, the ankle dorsiflexion remained 10° or less or the talar head was covered completely, and the hindfoot score was still >1.
For patients older than 30 months with persistent heel varus and forefoot supination following correction of other deformities, an anterior tibialis tendon transfer to the middle of the lateral cuneiform was done in theatre. It was done as an isolated procedure or with Achilles tenotomy if more than 10° of dorsiflexion could not be achieved. At the end of the treatment and just before the commencement of bracing, the passive foot abduction and dorsiflexion angles were taken with a goniometer, and the number of manipulations and castings required to achieve these were noted.
Technique for angular measurements (passive dorsiflexion and abduction)
Measurement of passive dorsiflexion: With the child supine, the knee flexed to 45° and the subtalar joint held in neutral to avoid including pronation in the measurement, the ankle is dorsiflexed maximally by pushing through the head of the fifth metatarsal. The axis of rotation is the intersection of the midline of the fibula and the midline of the fifth metatarsal. The stationary arm is placed in line with the fibular head, while the moving arm aligns with the fifth metatarsal as it is fully dorsiflexed. This angle is read off the goniometer.
Measurement of passive foot abduction: With the child supine and the knee flexed to 45°, the foot is placed with the centre of the heel on the goniometer underneath it. The stationary limb of the goniometer is in line with the sagittal plane of the tibia. The examining index finger is placed over the medial malleolus to stabilise the leg, and the ipsilateral thumb is placed over the lateral aspect of the talar head. The forefoot is then maximally abducted with the contralateral hand while at the same time positioning the measurement limb of the goniometer on the axis of the second toe. The angle is read off the goniometer.
The procedure was judged to have failed if after serial manipulation and casting for a maximum of 3 months without percutaneous tendoachilles tenotomy and/or anterior tibialis tendon transfer to the lateral cuneiform, a plantigrade foot with a Pirani score of 0 or 0.5 was not achieved.
Appropriately sized foot abduction brace (Iowa brace, Clubfoot Solutions, Coralville, Iowa, USA) was worn on children at full correction. In unilateral cases, the brace was set at 60–70° of external rotation on the clubfoot side and 30–40° on the normal side. In bilateral cases, 70° of external rotation on both sides was set. The brace was worn as follows: Twenty-three hours a day bracing for children <4 years old for the first three months, then nap and nighttime bracing until age 4. For those older than four years, night and nap time bracing for at least one year was done.
The derived data were analysed with the IBM SPSS® version 20 software. Results were presented in texts, tables, figures, and charts. Data were presented as means and standard deviations (SDs) for continuous variables. Categorical variables were presented as frequencies and percentages. Logistic regression was used to assess if the Pirani score at the presentation predicted successful treatment. The level of significance was set at P < 0.05.
Ethical clearance was obtained from the Institutional Ethics and Research Committee.
RESULTS
The Ponseti protocol had a success rate of 85.5% in the treatment of neglected clubfoot in this study. At the end of the study, out of the 69 feet recruited, 59 had a Pirani score of 0 or 0.5. These were judged to be successfully corrected, while those who scored above 0.5 were classified as treatment failures.
Age and the Pirani score(s) at presentation did not predict a successful treatment. However, the likelihood of a successful treatment had an inverse relationship with the Pirani score at presentation, but this was not statistically significant [Table 1 for results of the binary logistic regression analysis].
| Variable | β | S.E | P-value | 95% CI |
|---|---|---|---|---|
| Age | 0.001 | 0.027 | 0.978 | 0.949–1.055 |
| Pirani score at presentation | −0.485 | 0.305 | 0.112 | 0.338–1.120 |
S.E: Standard error, CI: Confidence interval, β:Probability of committing Type II error
The mean Pirani score at presentation was 4.27 (SD = 1.33), while the mean Pirani score at the end of manipulation and casting was 0.30 (SD = 0.35) [Figure 1].

- Line graph showing the change in the mean Pirani score at the end of casting.
The mean number of manipulation and casting sessions required to achieve correction of the deformity was 6.35 (SD = 1.95). There was a statistically significant correlation between the Pirani score at presentation and the number of casting sessions required for correction; r = 0.505, P < 0.001 [Figure 2].
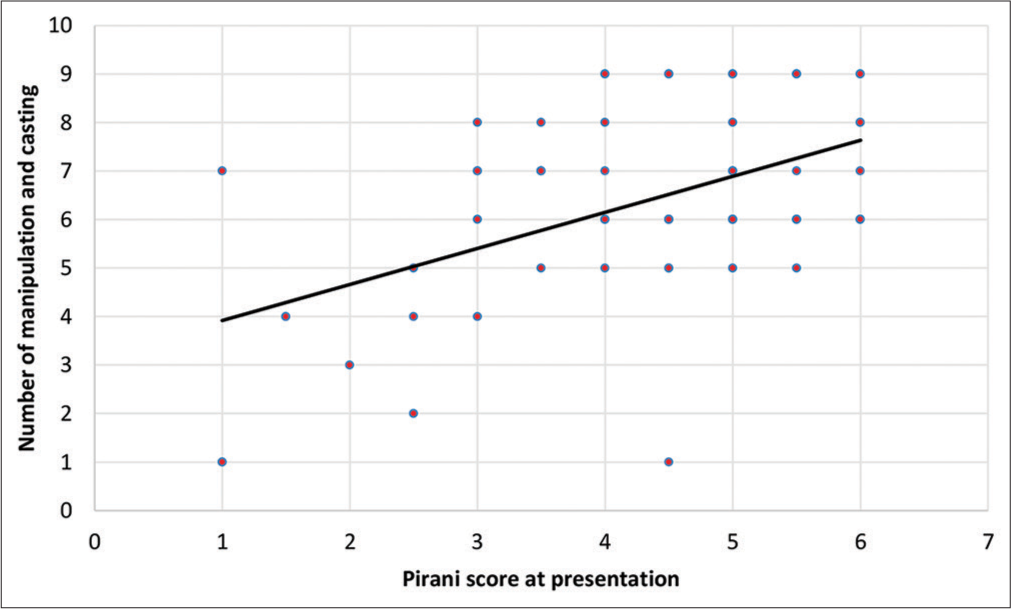
- A scatter plot showing a strong positive correlation between Pirani scores at presentation and the number of manipulations and casting required to correct the deformity.
Approximately half of the feet in this study had a previous unsuccessful non-operative treatment [Figure 3].
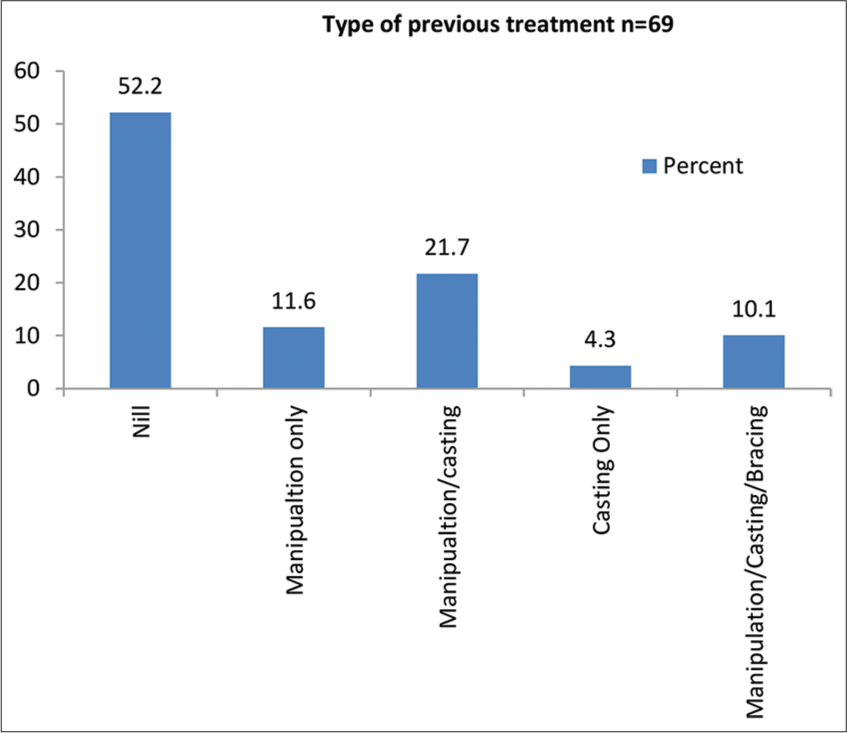
- The percentage of the feet that had previous non-operative treatment.
Bilateral involvement was the most common mode of presentation. Fifteen children had unilateral pathology; the right foot was involved in eight of them. Both feet were involved in 27 children [Figure 4].
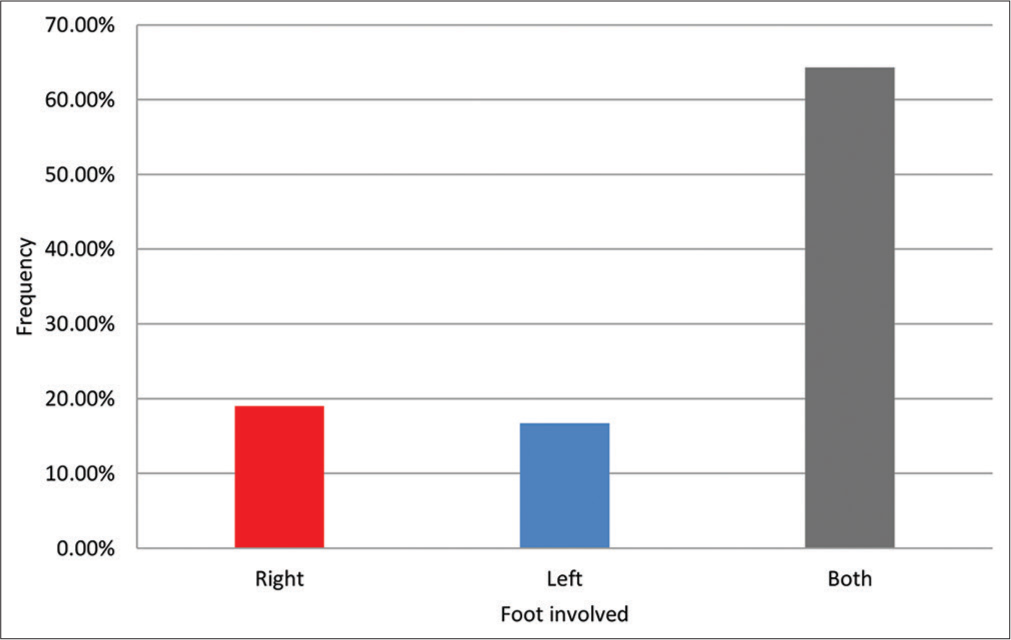
- The distribution of the feet affected in the study.
The male-to-female ratio was 3:1. The mean age of presentation was 27.45 months (SD = 19.22). The age range was 12–100 months. Most patients in the study presented in the 2nd and 3rd year of life (78.6%) [Table 2].
| Age categories (months) | N | % |
|---|---|---|
| 12–23 | 20 | 47.6 |
| 24–35 | 13 | 31.0 |
| 36–47 | 4 | 9.5 |
| ≥48 | 5 | 11.9 |
N: Frequency, %: Percentage frequency
DISCUSSION
The Ponseti method has been shown to be effective in the management of idiopathic CTEV. In this study, we are going to demonstrate that the Ponseti method is also efficacious in the treatment of neglected idiopathic CTEV.
The Ponseti method of treatment was successfully used to achieve the correction of neglected CTEV in 85.5% of the feet in this study. This is consistent with the works of Spiegel et al. and Adegbehingbe et al., who successfully treated 86% and 78% of feet, respectively.[2,8] Qureshi and Warriach, Lourenço and Morcuende, Ayana et al. had lower success rates with the Ponseti protocol in neglected CTEV.[5,6,9] Although the mean Pirani scores and the age range in their studies were similar to findings in this study, the average number of manipulation and casting was higher (8–9), and they ended up with a much lower success rate as only two-thirds of the feet treated had successful correction. They may have had a considerable number of rigid clubfeet in their study population. These feet although did not attain full correction, but the deformity was attenuated to require minimal soft tissue and bony surgeries for full correction. However, Tindall et al., Dargar et al., El-Banna and Meguid, and Sinha et al. documented higher success rates using the Ponseti method in the treatment of neglected CTEV with values in the range of 92–100%.[10-13] The patients treated by El-Banna and Meguid were relatively younger (mean age of 16. 3 months), as well as those treated by Tindal et al. who had only 25% of their patients in the age range 18–48 months as part of a larger study of 75 patients (100 feet).[11,13] This relatively younger age group may explain their higher rate of success compared to our findings. Dargar et al. and Sinha et al. successfully treated 100% of their patients and had an age range of 1–10. For three years, their average Pirani scores at presentation (5 and 5.4, respectively) mirrored that of our study, but they did more sessions of manipulation and casting (9 and 12.8 sessions) in that order.[10,12] A study revealed that the higher the casting sessions the odds of ambulating with deformity reduces.[1]
The Pirani score(s) at the presentation did not predict a successful treatment. This finding may be the result of previous inappropriate or inadequate treatment(s) received by some of the patients (approximately half of the study population), weight-bearing contributing to stretching of the foot soft tissues, or the relative atrophy of the affected limbs, all resulting in a flexible foot. Furthermore, the Pirani score as an assessment tool for neglected CTEV commonly gives lower values. This limitation is occasioned by the obliteration of the medial and posterior creases with weight bearing and the decrease in the empty heel pad due to the usual loss of subcutaneous fat with growth, thus giving relatively lower scores with aging.[5,8]
At presentation, the mean Pirani score was slightly lower than the average Pirani score of the reviewed literature. This may likely be the effect of previous unsuccessful nonoperatively treated patients included in the study sample. These children had a milder deformity compared to their counterparts who had yet to receive any form of treatment as at the time of presentation. At the end of treatment, the mean Pirani score in this study was relatively higher compared to the post treatment Pirani score of 0.21 reported by an Indian study.[12] However, it was lower than the values recorded by studies from Egypt, Nepal and Pakistan which recorded 0.9, 2.1 (SD = 1.03) and 1.31 (SD = 0.43), respectively.[8,9,11]
The mean number of manipulation and casting sessions needed to achieve correction in this study was comparable to the findings reported by Nigerian, other African and Asian studies,[2,5,8,11,13] while some other studies reported relatively higher scores.[6,9,10,12] This may be accounted for by the slightly lower mean Pirani scores at presentation recorded in this study.
In this study, two patients with three affected feet (4.3%) required transfer of the anterior tibialis tendon (ATTT) to the lateral cuneiform to correct a dynamic forefoot supination noted at the end of serial manipulation and casting. El-Banna and Meguid performed ATTT in 24% of their patients, a value much higher in comparison to this study.[11] The upside of this finding is that all the procedures required to obtain correction in most of the patients were done outside of the operating room in this study.
Our study revealed that bilateral cases accounted for about two-thirds of the patients. This presentation was similar to another Nigerian study.[1] But different from what is recorded in the literature where bilateral cases accounted for about half of the patients.[2,5,14] The observed difference may have resulted from failure by parents/guardians to initiate or complete treatment (if at all it was sort for) due to double the financial cost of treatment materials when compared with unilateral cases. Furthermore, parents and caregivers of bilateral cases may have presented in higher proportion given more difficulty experienced by their children or wards during walking. This could also signify a changing demography of presentations.
In our study, there was male preponderance which was approximately equal to the global figure. The perceived slight increase in male patients with neglected clubfoot who presented to the hospital may have been due to the following reasons. First, a major factor may be the male preponderance in the global incidence of CTEV in general. In addition, many parents in our environment place more value on the cosmesis of their female children, which they believe will increase their chances at marriage, thereby presenting early to the hospital for care, thus reducing the prevalence of neglect in them and leaving mostly males to bear this burden. However, in some communities that hardly ever seek medical care for this deformity, late presentation may be the order of day generally, and since males enjoy higher enrolment rates into school, they may have presented on account of peer pressure. This male preponderance is also seen in the works done by Adegbehingbe et al., Qureshi and Warriach, El-Banna and Meguid, although to a lesser degree compared to this study, which led Adegbehingbe et al. to conclude that there was no gender bias in the presentation of neglected clubfoot cases in their series.[2,9,11]
The age range of children in this study was 12–100 months (8 years). This age bracket was similar to studies done by numerous researchers. The youngest child was one year old, in line with the inclusion criteria. Ayanna et al.,[5] Lourenco et al.,[6] Dargar et al.,[10] Spiegel et al.,[8] and Sinha et al.[12] all had a similar age range of 1–10 years.[5,6,8,10,12] Likewise, Adegbehingbe et al. had 91.5% of their study group with an age range of 1–9 years; the oldest child in their work was 16 years.[2]
CONCLUSION
The Ponseti method can be used for the treatment of neglected idiopathic congenital talipes equinovarus deformity with a high success rate. Therefore, it is recommended as the first line of treatment for neglected CTEV.
The age of the children and their Pirani scores at presentation did not predict the likelihood of a successfully corrected neglected idiopathic CTEV using the Ponseti method.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Management of club foot using Ponseti technique: Assessment of treatment outcomes and their determinants. Afr J Paediatr Surg 2023 doi: 10.4103/ajps.ajps_115_22
- [CrossRef] [Google Scholar]
- Ponseti method treatment of neglected idiopathic clubfoot: Preliminary results of a multi-center study in Nigeria. World J Orthop. 2017;8:624-30.
- [CrossRef] [PubMed] [Google Scholar]
- The neglected clubfoot In: Techniques in orthopaedics. Vol 2. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. p. :153-66.
- [CrossRef] [Google Scholar]
- Gross motor development of Nigerian children. Ann Trop Paediatr. 1991;11:33-9.
- [CrossRef] [PubMed] [Google Scholar]
- Good results after Ponseti treatment for neglected congenital clubfoot in Ethiopia. A prospective study of 22 children (32 feet) from 2 to 10 years of age. Acta Orthop. 2014;85:641-5.
- [CrossRef] [PubMed] [Google Scholar]
- Correction of neglected idiopathic clubfoot by the Ponseti method. J Bone Joint Surg Br. 2007;89:378-81.
- [CrossRef] [PubMed] [Google Scholar]
- Controversies in congenital clubfoot: Literature review. Malays J Med Sci. 2002;9:34-40.
- [Google Scholar]
- Ponseti method for untreated idiopathic clubfeet in Nepalese patients from 1 to 6 years of age. Clin Orthop Relat Res. 2009;467:1164-70.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of Ponseti method for management of idiopathic clubfoot in toddlers. Pak J Med Sci. 2013;7:730-2.
- [Google Scholar]
- Results of Ponseti treatment in clubfoot in older children in India. Int J Sci Res (Ahmedabad). 2015;4:547-8.
- [Google Scholar]
- Evaluation of the Ponseti technique in the management of clubfoot in older children. Med J Cairo Univ. 2012;80:205-17.
- [Google Scholar]
- Evaluation of Ponseti method in neglected clubfoot. Indian J Orthop. 2016;50:529-35.
- [CrossRef] [PubMed] [Google Scholar]
- Results of manipulation of idiopathic clubfoot deformity in Malawi by Orthopaedic clinical officers using the Ponseti method: A realistic alternative for the developing world? J Pediatr Orthop. 2005;25:627-9.
- [CrossRef] [PubMed] [Google Scholar]
- Experience with accelerated Ponseti technique for treatment of idiopathic clubfoot in a regional orthopaedic hospital in Nigeria. Afr J Paediatr Surg. 2023;20:106-8.
- [CrossRef] [PubMed] [Google Scholar]






