Translate this page into:
Metachromatic leukodystrophy (MLD) presenting as initial cognitive regression and myoclonic epilepsy with normal magnetic resonance imaging (MRI) of the brain
*Corresponding author: Vykuntaraju K. Gowda, Department of Pediatric Neurology, Indira Gandhi Institute of Child Health, Bengaluru, Karnataka, India. drknvraju08@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gowda VK, Babu S, Srinivasan VM. Metachromatic leukodystrophy (MLD) presenting as initial cognitive regression and myoclonic epilepsy with normal magnetic resonance imaging (MRI) of the brain. Karnataka Paediatr J. 2024;39:155-6. doi: 10.25259/KPJ_35_2024
Abstract
Metachromatic leukodystrophy (MLD) is a rare disorder due to mutations in the ARSA gene leading to arylsulfatase A deficiency. We present a case of late infantile onset MLD with a novel phenotype. A 5-year-old boy presented with myoclonic jerks and tonic seizures from two years of age followed by initial cognitive and later motor regression. On examination, horizontal nystagmus, spasticity with power >3/5 in all limbs, and sluggish deep tendon reflexes were noted. MRI brain done at 2, and 5 years were normal. Exome sequencing showed compound heterozygous variants in ARSA: NM_0010854 25.3: c.433C>T: p. Arg145Ter (exon 3) and c.902G>A: p. Arg301Gln (exon-5) classified as pathogenic and likely pathogenic as per ACMG classification respectively and segregated with the disease in the family. Arylsulfatase A was low: 0.25nmol/hr/mg protein (normal range 0.6-5.0). To conclude MLD can have normal neuroimaging even at 5 yr. with atypical initial cognitive regression.
Keywords
Metachromatic Leukodystrophy
Progressive myoclonic epilepsy
Cognitive regression
INTRODUCTION
Metachromatic leukodystrophy (MLD) is a rare disorder due to mutations in the arylsulfatase A (ARSA) gene leading to arylsulfatase A deficiency.[1] We present a case of late infantile onset MLD with a novel phenotype.
CASE REPORT
A 5-year-old boy presented with myoclonic jerks and tonic seizures from 2 years of age, followed by initial cognitive and later motor regression. Loss of meaningful language output, comprehension, and ability to drink and feed by himself after the onset of seizures. The child developed stereotypes in the past 6 months. On examination, horizontal nystagmus, spasticity with power >3/5 in all limbs, sluggish ankle jerk, and normal in the other deep tendon reflexes were noted. Magnetic resonance imaging (MRI) brain done at 2, and 5 years were normal [Figure 1]. Tandem mass spectroscopy and enzyme for neuronal ceroid lipofuscinosis (NCL) 1 and 2 were normal. Exome sequencing showed compound heterozygous variants in ARSA: NM_0010854 25.3: c. 433C>T: p. Arg145Ter (exon 3) and c.902G>A: p. Arg301Gln (exon-5) classified as pathogenic and likely pathogenic as per ACMG classification, respectively, and segregated with the disease in the family. Arylsulfatase A was low: 0.25 nmoL/h/mg protein (normal range 0.6–5.0).
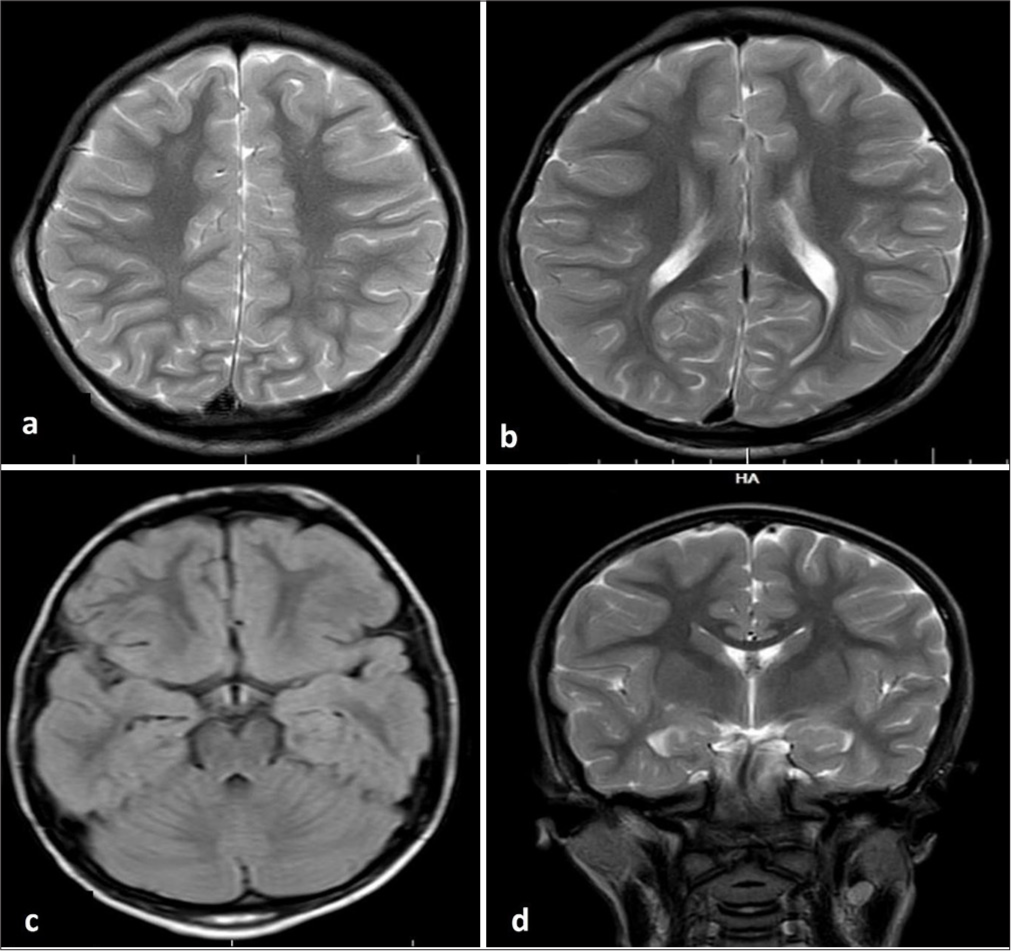
- (a-d) Magnetic resonance imaging of the brain not showing any abnormalities.
DISCUSSION
Differentials considered were NCL and gangliosidosis. The neuroimaging in MLD is usually abnormal except for the late infantile form, where the initial scans may be normal or have minimal changes.[2,3] The neuroimaging anomalies in these cases were estimated to be seen at the breakpoint of 1.75 years.[2,4] However, repeat neuroimaging at 5 years was also normal in the current case. Normal MRI may mislead and delay the diagnosis of MLD and, in turn, the period for genetic counselling. The possible explanations for normal neuroimaging are the presence of immature myelin, signs of neuropathy leading to neurological symptoms, enzyme levels and genetic factors.[2]
CONCLUSION
MLD can have normal neuroimaging even at 5 years with atypical initial cognitive regression.
Ethical approval
Institutional Review Board has waived the ethical approval for this study
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Histopathologic correlates of radial stripes on MR images in lysosomal storage disorders. AJNR. 2005;26:442-6.
- [Google Scholar]
- Recognizing early MRI signs (or their absence) is crucial in diagnosing metachromatic leukodystrophy. Ann Clin Transl Neurol. 2022;9:1999-2009.
- [CrossRef] [PubMed] [Google Scholar]
- Metachromatic leukodystrophy: Natural course of cerebral MRI changes in relation to clinical course. J Inherit Metab Dis. 2011;34:1095-102.
- [CrossRef] [PubMed] [Google Scholar]
- T2-Pseudonormalization and microstructural characterization in advanced stages of late-infantile metachromatic leukodystrophy. Clin Neuroradiol. 2021;31:969-80.
- [CrossRef] [PubMed] [Google Scholar]







