Translate this page into:
Salmonella typhimurium meningitis in an exclusively breast fed infant: A case report
*Corresponding author: H. R. Sanjay, Department of Paediatrics, Father Muller Medical College, Mangalore, Karnataka, India. sanjayhosamane@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sanjay HR, Avabratha KS, Alva R. Salmonella typhimurium meningitis in an exclusively breast fed infant: A case report. Karnataka Paediatr J 2021;36:135-7.
Abstract
Salmonella-related meningitis brings greater morbidity and mortality than that caused by other bacteria. We report a case of Salmonella typhimurium meningitis in a male child aged 5½ months who presented with fever, poor feeding, and irritability. Anterior fontanelle was bulged. S. typhimurium was isolated from cerebrospinal fluid. Child was treated with intravenous antibiotics for 4 weeks and he recovered completely.
Keywords
Infant
Salmonella typhimurium
Meningitis
INTRODUCTION
Salmonella meningitis is rare and is prevalent mostly among infants and young children.[1] Bacteraemia and other forms of extra-intestinal salmonella infection are serious complications. Salmonella-related meningitis brings greater morbidity and mortality than that caused by other bacteria.[2] Due to salmonella meningitis, mortality rates of 40% are recorded in infants.
Among survivors, epilepsy, hydrocephalus, subdural empyema, and permanent disabilities such as retardation, paresis, athetosis, and visual defects are the common complications.[1] Here, we report a 5½-month-old infant successfully managed with longer duration of intravenous antibiotics.
CASE REPORT
Five and half months exclusively breast fed male infant presented with complaints of fever, irritability, and poor feeding of 1 day duration. There was no history of respiratory and gastrointestinal symptoms. General examination showed irritable cry, bulged anterior fontanelle with GCS of 10/15. Baby weighed 7.5 kg. Central nervous system examination showed hypertonia of all four limbs, exaggerated reflexes. Blood investigations showed normocytic normochromic anaemia with pancytopenia (Hb: 9.1 g%, WBC: 2600/mm3, and Platelet count: 120,000/mm3). Child developed repeated seizures on the day of admission, hence loaded on IV Levetiracetam after 2 doses of midazolam and meningitis dose of ceftriaxone was started. Lumbar puncture revealed a slightly turbid cerebrospinal fluid with a total count of 400 cells/cumm, Neutrophils – 60%, and Lymphocytes – 40%. Cerebrospinal fluid protein was elevated to 316.2 mg/dl and sugar was 22 mg/dl. Cerebrospinal fluid and blood culture showed growth of Salmonella typhimurium sensitive to Amoxicillin-clavulanic acid, Ceftriaxone, Co-trimoxazole, Ceftazidime, Piperacillin-tazobactam, Meropenem and resistant to Amikacin, Gentamicin, and Cefazolin. Mother’s stool showed growth of S. typhimurium. Both parents were treated with ciprofloxacin. Child continued to have seizures hence additional anti-epileptics (Fosphenytoin and sodium valproate) were added. In view of persisting thrombocytopenia, anaemia and altered sensorium neurosonogram was done to rule out any intracranial bleeds, which was normal. Electroencephalogram was normal. In bilateral cerebral hemispheres, MRI brain displayed acute infarctions [Figure 1]. After obtaining culture and sensitivity pattern on day 4, child was started on IV ciprofloxacin.
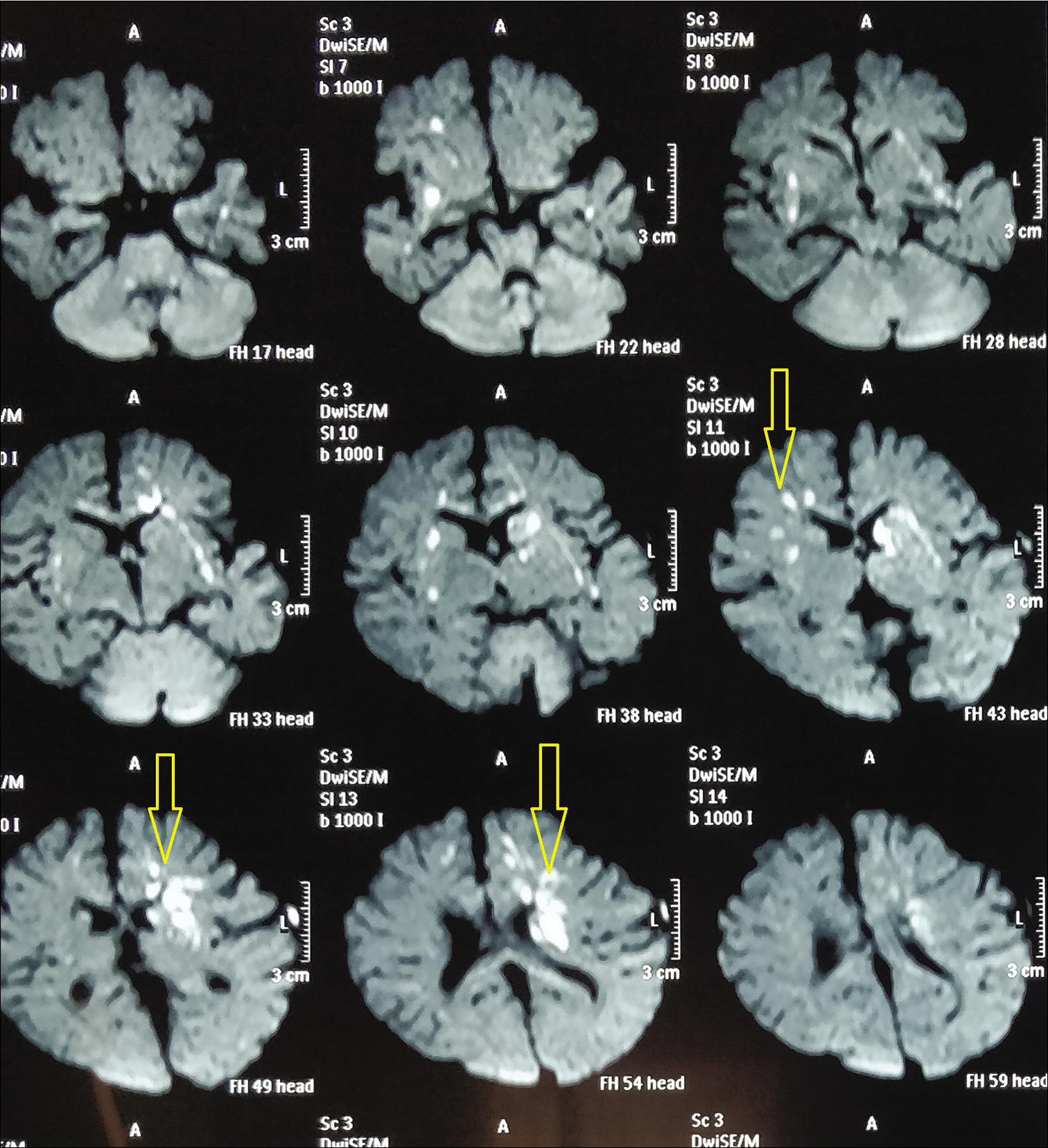
- Acute infarcts in bilateral cerebral hemispheres.
The infant was treated with ceftriaxone intravenously for 4 weeks and ciprofloxacin intravenously for 2 weeks. Child improved gradually. By day 5 children had no further convulsions; tube feeds were initiated and gradually increased as tolerated. By day 9 sensorium of the child improved, face regard was present; sucking well was started on direct breast feeds. IV anti-epileptic drugs were made oral and tapered one by one. By day 16, child was transferred to ward and IV ceftriaxone was continued for 28 days. By day 29 children recovered completely and were discharged with stable vitals. Child is being followed up regularly and development is normal. Repeat EEG done after 6 months was normal and hence anticonvulsants were stopped.
DISCUSSION
It is considered that acute bacterial meningitis is a medical emergency that needs early detection and aggressive care. Very commonly, bacterial meningitis care must be started before the etiology is identified.[3]
S. typhimurium is a facultative aerobic, Gram-negative bacterium, which often infects cattle and poultry which often are the sources of infection in humans. Beyond the neonatal period meningitis due to S. typhimurium is uncommon. In infants and adults, sporadic cases of pyogenic meningitis caused by S. typhimurium have been reported.[4-8] Salmonella enteritidis was the most common serotype isolated from positive CSF cultures in 4-month-old infants in a retrospective analysis study by Lee et al.[9]
Antibiotic regimens for salmonella meningitis treatment in children always remained uncertain. In the treatment of facultative intracellular species, such as salmonellae, a combination of third-generation cephalosporin and gentamicin, widely used for the treatment of meningitis due to gram-negative enteric bacilli, may not be appropriate. The consideration of antibiotic therapy with a combination of ciprofloxacin and ceftriaxone/cefotaxime for Salmonella meningitis was suggested by Price et al.[10] Although the use of ciprofloxacin in children has raised questions about arthropathy, it is highly rare and can be used in the treatment of severe paediatric infections where the possible benefits outweigh the risks.[11] One research recommended a high dose of third-generation cephalosporin for at least 4 weeks to ensure that Salmonella meningitis is treated successfully and to avoid relapse.[12] Same regimen was followed in our case which had good outcome.
S. typhimurium in immunocompetent infants worldwide, including in India, is a rare cause of acute bacterial meningitis.[13] Most common mode of transmission is feco-oral. In the family members of patients who are asymptomatic reports on Salmonella surveillance are rare. However, the suspicion of Salmonella infection must be raised when there might be a carrier of Salmonella among family members. The pathogen may readily be transmitted from mother to child as the mother has the most contact with an infant.[14] The source of infection was mother in our case. Hence, it is important to find the source of infection and treat accordingly if parents or other family members are infected.
CONCLUSION
Every effort should be made to culture causative organism in meningitis. S. typhimurium meningitis, though rare should be considered in infants. Prompt treatment with third generation cephalosporin for prolonged period is necessary for good outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Salmonellosis. In: Fauci AS, Braunwald E, Isselbacher KJ, Wilson JD, Martin JB, Kasper DL, eds. Harrison's Principles of Internal Medicine (14th ed). New York: McGraw-Hill; 1998. p. :950-6.
- [Google Scholar]
- Neonatal meningitis caused by Salmonella enterica with multiple brain abscess: A case report. Kuwait Med J. 2010;42:74-6.
- [Google Scholar]
- Bacteriological profile of community acquired acute bacterial meningitis: A ten-year retrospective study in a tertiary neurocare centre in South India. Indian J Med Microbiol. 2007;25:108-14.
- [CrossRef] [Google Scholar]
- Salmonella typhimurium meningitis in a five-month-old infant. Kuwait Med J. 2003;36:45-6.
- [Google Scholar]
- Acute bacterial meningitis in children admitted to the Queen Elizabeth Central Hospital, Blantyre, Malawi in 1996-97. Trop Med Int Health. 1998;3:610-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal Salmonella typhimurium meningitis. Indian J Pediatr. 2001;68:1079-80.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella typhimurium brain abscess in a six-month-old infant: A case report and review of the literature. Changgeng Yi Xue Za Zhi. 1997;20:219-25.
- [Google Scholar]
- Salmonella typhimurium meningitis in an adult patient with AIDS. Clin Pathol. 2008;61:138-9.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella meningitis and its complications in infants. J Paediatr Child Health. 1999;35:379-82.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotics for Salmonella meningitis in children. J Antimicrob Chemother. 2000;46:653-5.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella typhimurium meningitis in an immunocompetent infant. Indian J Case Rep. 2017;3:252-4.
- [CrossRef] [Google Scholar]
- Persistence of Salmonella species in cerebrospinal fluid in patient with meningitis following ceftriaxone therapy. Clin Infect Dis. 1999;28:1174-5.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic nontyphoidal Salmonella infection in normal infants in Thailand. Pediatr Infect Dis J. 2001;20:581-7.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella meningitis: A report from National Hue Central Hospital, Vietnam. Jpn J Infect Dis. 2015;68:30-2.
- [CrossRef] [PubMed] [Google Scholar]






