Translate this page into:
Status dystonicus in children: Treat the precipitating factors
*Corresponding author: Lokesh Saini, Department of Pediatric Neurology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. drlokeshsaini@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Madaan P, Bhanudeep S, Saini L. Status dystonicus in children: Treat the precipitating factors. Karnataka Paediatr J 2021;36(1):54-6.
Abstract
Status dystonicus (SD) is a life-threatening movement disorder associated with significant morbidity and requires immediate and urgent intervention. It usually develops from both primary and secondary dystonias and rarely can be a complication of symptomatic insults such as infections, brain insults, or drugs. Compared to adults, it is seen more commonly in children due to the risk of many trigger factors and vulnerability of the developmental brain. Due to the delay in the identification and prevention of the triggering factors, nowadays most children require intensive care. Here, we report a 1-year-old boy, who was a known case of dyskinetic cerebral palsy, presented with increased twisting movements after an episode of febrile illness. The SD partially resolved after midazolam infusion, however, after treating the triggering factors (constipation and pneumonia), the SD resolved completely.
Keywords
Status dystonicus
Kernicterus
Dyskinetic cerebral palsy
INTRODUCTION
Status dystonicus (SD) was first described by Jankovic and Penn as “an uncommon neurological emergency with acute worsening of dystonia requiring urgent hospital admission.” It is called by various other names such as dystonic storm, life-threatening dystonia, and desperate dystonic. Dystonia usually worsens as a continuum spectrum ranging from pre SD to SD. Different drugs had been used to alleviate dystonia through muscular relaxation, sleep sedation, and reduction of pain due to muscular contraction. However, unless the precipitating factor is taken care of, the status dystonia does not resolve and may progress to severe rhabdomyolysis. We here, describe a 1-year-old boy presenting with severe SD and subsided after treating the precipitating factors.
CASE REPORT
A 1-year-old boy presented with fever, increased work of breathing, and increased twisting posturing episodes each lasting for 30 min to 1 h for the past 4 days. The child was born at term with a smooth perinatal transition. There was a history of jaundice on day 2 of the birth with bilirubin levels maximum up to 40 mg/dl. He required double-volume exchange transfusion and phototherapy with which jaundice resolved. He had partial neck control, recognizes mother but cannot sit with support, and also does not respond to auditory stimuli. He also developed choreoathetoid movements of bilateral upper and lower limbs at 6 months of age. The child had a history of constipation since infancy which had worsened over the past week. There was no history of seizures, recurrent respiratory tract infections, or persistent vomiting. Examination revealed microcephaly, bilateral spasticity with severe opisthotonic posturing, brisk deep tendon reflexes, bilateral upgaze palsy, positive Babinski sign, and palpable fecoliths on the abdomen. The child was diagnosed as dyskinetic cerebral palsy (CP) with SD with community-acquired pneumonia. Investigations revealed elevated creatine kinase (8573 U/L) and lactate dehydrogenase (567 U/L). Neuroimaging revealed bilateral symmetrical globus pallidus hyperintensities [Figure 1]. He was started on antipyretics, empirical antibiotics (Ampicillin and Gentamicin), and anti-dystonic drugs such as trihexyphenidyl, clonazepam, melatonin, baclofen, and midazolam infusion. His dystonia did not resolve even after 24 h after starting midazolam infusion. He was given lactulose syrup along with polyethylene glycol with which the constipation was relieved. Within the next few hours, the SD resolved. We could gradually wean the child from ventilator and make him off sedation. His biochemical parameters such as creatine kinase and lactate dehydrogenase were also normalized.
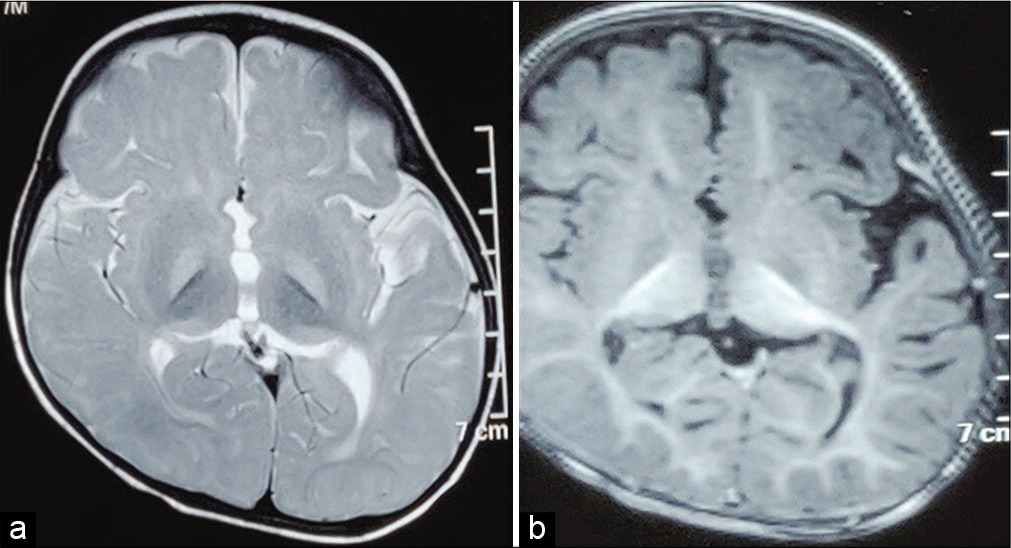
- Neuroimaging of the index child. (a) T2-weighted image showing bilateral symmetrical globus pallidus hyperintensity (b) T1-weighted image showing bilateral globus pallidus hypointensity.
DISCUSSION
SD is characterized by frequent and severe episodes of generalized dystonia with significant morbidity and requires immediate and effective treatment. It can be either primary (DYT1) or secondary to infections, perinatal insult, trauma, or drugs.[1] Some children with genetic or acquired underlying conditions are prone to develop SD. The acquired causes such as dyskinetic CP are the most common to cause SD. Various genetic causes such as infants with ARX mutation and GNAO1-related epileptic encephalopathy can also develop SD.[1,2] Dyskinetic CP secondary to kernicterus continues to be an unfortunate but preventable occurrence in developing countries. Early markers of evolving dyskinetic CP such as upgaze palsy and rhythmic tongue thrusting need to be stressed to prevent the delay in the initiation of rehabilitation.[2-4] These early markers can help in early diagnosis and institution of early intervention before 6 months of age when surround inhibition and selective control have not yet developed and overt dystonia are not evident.[5,6] This is the probable reason for SD being a rarity in infants with evolving CP; although it may be seen in progressive neurological conditions in infancy.
The term “prestatus dystonicus” has been proposed for an immediately preceding step in the deterioration of acute or subacute dystonia. Hence, early recognition and intervention in the pre SD step are crucial in the acute management to prevent progression to SD and its complications.[1,2] Management of SD is considerably different in infants and children when compared to adults where there are various treatment options such as anti-dystonic drugs such as trihexyphenidyl, syndopa, and tetrabenazine, sedative drugs such as benzodiazepines, deep brain stimulation, and pallidotomy.[2,3] However, in infants and children, the precipitating or trigger factors need to be addressed appropriately along with medical management. The common precipitating factors include infections (gastroenteritis with dehydration, and upper and lower respiratory tract infections), painful stimuli, constipation, poor handling of secretions, gastroesophageal reflux, chelation therapy with D-Penicillamine, zinc sulfate, and trauma.[3,4] These precipitating factors lead to a vicious cycle with worsening dystonia and this cycle can only be broken down by targeting the precipitating factors. Only running behind dystonia is not a fruitful strategy in SD. In the index child both the pneumonia and constipation precipitated SD and the dystonia resolved after treating the precipitating factors.
Ethical statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Authors’ contribution
PM and BS: Literature review, and initial draft manuscript preparation; LS: Critical review of manuscript for important intellectual content. All authors approved the final version for publication.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Status dystonicus: Management and prevention in children at high risk. Acta Biomed. 2019;90:207-12.
- [Google Scholar]
- Prestatus and status dystonicus in children and adolescents. Dev Med Child Neurol. 2020;62:742-9.
- [CrossRef] [PubMed] [Google Scholar]
- Gaze palsy: An important diagnostic clue. J Pediatr. 2019;212:236.
- [CrossRef] [PubMed] [Google Scholar]
- Rhythmic tongue thrusting: A useful clinical sign. Pediatr Neurol. 2020;102:81-2.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral palsy: Early markers of clinical phenotype and functional outcome. J Clin Med. 2019;8:1616.
- [CrossRef] [PubMed] [Google Scholar]
- Recognizing the common origins of dystonia and the development of human movement: A manifesto of unmet needs in isolated childhood dystonias. Front Neurol. 2016;7:226.
- [CrossRef] [Google Scholar]






