Translate this page into:
Eschar in scrub typhus
*Corresponding author: Vykuntaraju K. Gowda, Department of Pediatric Neurology, Indira Gandhi Institute of Child Health, Bengaluru, Karnataka, India. drknvraju08@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy SC, Gowda VK, Kinhal UV, Srinivas SM. Eschar in scrub typhus. Karnataka Paediatr J. 2024;39:68-9. doi: 10.25259/KPJ_4_2024
Dear Editor,
Rickettsial diseases are caused by a variety of obligate intracellular, Gram-negative bacteria from the genera Rickettsia, Orientia, Ehrlichia and Anaplasma.[1].Rickettsial infections are underdiagnosed in India due to their non-specific clinical presentation.[2] The presence of an eschar, less commonly observed in the Indian population, contributes to the diagnostic process. Therefore, we are sharing this image to create more awareness of this treatable life-threatening condition.
A 2-year-old female child presented with a fever lasting seven days and seizures on day 6 of fever. On examination, vital signs were stable, revealing three eschars: One over the mid back adjacent to the medial border of the left scapula [Figure 1a], over the back below the right scapular region [Figure 1b] and the third over the left mastoid region [Figure 1c]. On systemic examination, a Glasgow Coma Scale of 5/15, meningeal irritations, brisk deep tendon reflexes and hepatosplenomegaly were noted. Investigations revealed a total leukocyte count of 18700/mm3, haemoglobin of 10.7g/dL, platelet count of 44000/mm3, total protein of 4.2 g/dL, serum albumin of 1.8g/dL, aspartate aminotransferase of 279.3U/L, alanine aminotransferase of 123.1U/L, serum urea of 122.9 mg/dL and serum creatinine of 0.86 mg/dL. The Weil Felix test was positive for OXK (1:320). Serum and cerebrospinal fluid immunoglobulin M enzyme-linked immunosorbent assay were positive for Orientia tsutsugamushi. Work-up for other infections, such as dengue and malaria, was negative. The child was treated symptomatically and with oral doxycycline for seven days, leading to improvement in the child’s condition. Rickettsial eschars are necrotic lesions that occur at the site of tick or mite bites and represent locations of primary inoculation of spotted fever group Rickettsia and Orientia species.[3] A rickettsial eschar begins as a small, painless papule that appears within a few days after the bite of an infected vector. The papule grows, becomes vesicular or pustular and ulcerates, forming a brown-to-black crust surrounded by a red annular halo. The presence of an eschar can aid in the clinical and epidemiologic differentiation of less severe spotted fever rickettsioses from the more severe Rocky Mountain spotted fever. Rickettsial eschars serve as an important clinical specimen.[3]
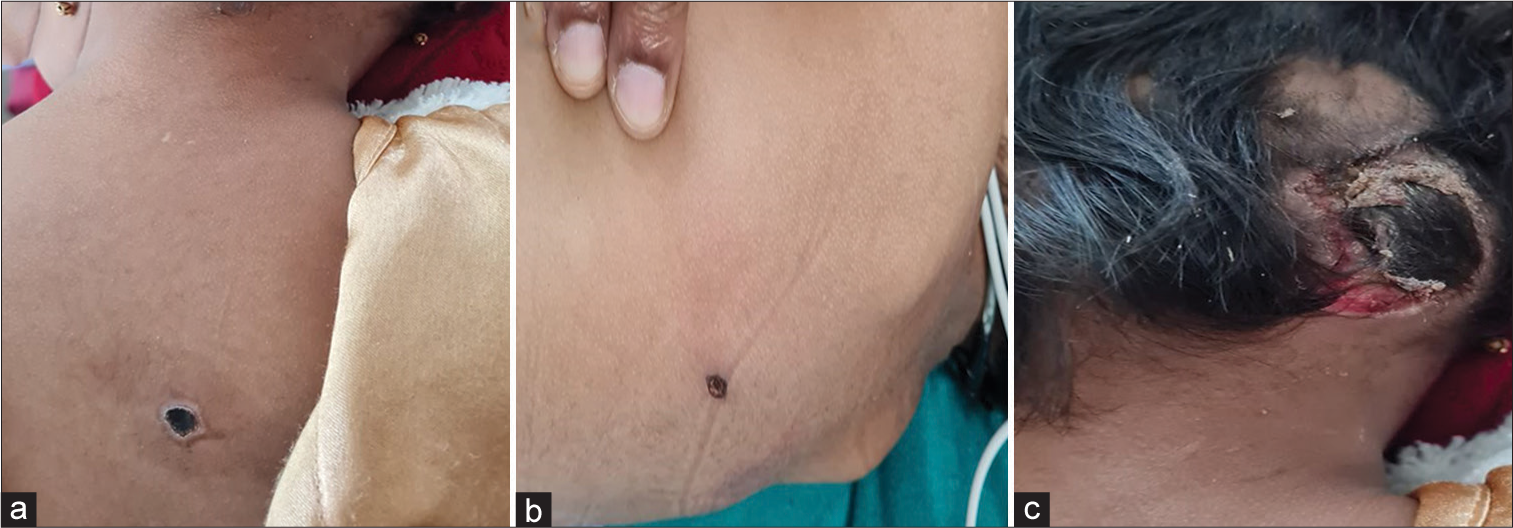
- (a) An eschar over the mid back adjacent to the medial border of the left scapula with a black adherent crust surrounded by an erythematous halo, (b) an eschar over the back below the right scapular region with a characteristic black crust and (c) an eschar over the left mastoid region with a black necrotic crust.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Rickettsioses in children-a review. Indian J Pediatr. 2020;87:930-6.
- [CrossRef] [PubMed] [Google Scholar]
- Rickettsial infection in children-clinical profile and response to treatment. MedPulse Int J Pediatr. 2021;18:1-5.
- [CrossRef] [Google Scholar]
- Description of Eschar-associated Rickettsial diseases using passive surveillance data-United States, 2010-2016. MMWR Morb Mortal Wkly Rep. 2020;68:1179-82.
- [CrossRef] [PubMed] [Google Scholar]





